Authors:
Melony Chakrabarty MD and Archana Maniar MD
UC-Davis Medical Center
A 70yr old Hispanic male with presents with history of disseminated coccidioidomycosis diagnosed in 2004 with progression of disease in 2016 with basilar meningitis requiring ventriculoperitoneal shunt. He has been on Voriconazole 200mg BID since June 2016, and has had therapeutic Voriconazole levels since 8/2016 (ranging 2.6 – 5.1). Admitted February 2018 for acute on chronic weakness occurring after a fall 2-3 months ago where he lost coordination and tripped over a table. Noted joint pain over L shoulder, L elbow and 2nd and 3rd L metacarpals. He describes the pain as an aching sensation with stiffness and is no longer to extend his elbow fully and he now requires assistance with walker for ambulation. ROS is notable for no headache, neck pain, fever, chills or weight loss.
Of note, he had outpatient evaluation 10/2017 for lytic bone lesions including biopsy of L iliac bone and bone marrow biopsy which were inconclusive.
PMH:
- Diabetes (HgBA1c 9.8%)
- Pulmonary embolism and Deep Venous Thrombus
- Hyperlipidemia
SH: Lives in north-central California, previously was farmer. Prior tobacco use, no other IVDU or alcohol use
Allergies: NKDA
Current medications: voriconazole 200mg BID, atorvastatin, rivaroxaban, glimepiride, metformin
Physical Examination:
VS: 36.8 C T, BP 126/81, HR 76, RR 18, SpO2 98% on RA
General: Well appearing, no acute distress, normal speech
HEENT: EOMI, PERRLA, normal dentition and no tongue ulcers noted
CV: Regular rate and rhythm, no murmur, 2+ radial pulses bilaterally
Resp: Clear to auscultation bilaterally
Abd: No hepatosplenomegaly, soft, nontender
MSK: 2nd/3rd L MCP with bony enlargement, tender on passive ROM, no appreciable effusion. L elbow stiffness and decreased range of motion (unable to flex past 120 degrees) no palpable bone growths over olecranon process, unable to abduct shoulder past 75 degrees
Neuro: cranial nerves intact, strength 5/5 with decreased ROM as noted above, no nuchal rigidity
Skin: Thin skin with loss of skin folds on fingers
Laboratory Examination:
Electrolytes and hematology values were normal.
Alk Phos 185 U/L – mildly elevated
AST 14 U/L – normal
ALT 12 U/L – normal
Tbili 0.6 mg/dL – normal
Voriconazole level 2.6 µg/mL
Microbiology:
10/2017 Fungal tissue culture and histopathology from L iliac bone biopsy: negative
Cocci serologies
Serum: 6/2016 1:256 11/2016 1:128 7/2017 1:32 11/2017 1:64
CSF: 6/2016 1:256 9/2016 1:64 12/2016 1:128 5/2017 1:32
Imaging:
MRI spine: Mottled heterogenous signal intensity of the vertebral bodies, enhancing lesion of L4 stable from prior imaging
Plain films of shoulder, elbow and hand: Diffuse osteopenia with mottled appearance, endosteal scalloping involving shoulder and elbow. Hand film notable for radiodensities over soft tissue of second and third digit and periarticular osteopenia.
Bone scan: periosteal process with uptake in proximal limbs, posterior pelvis and posterior central ribs
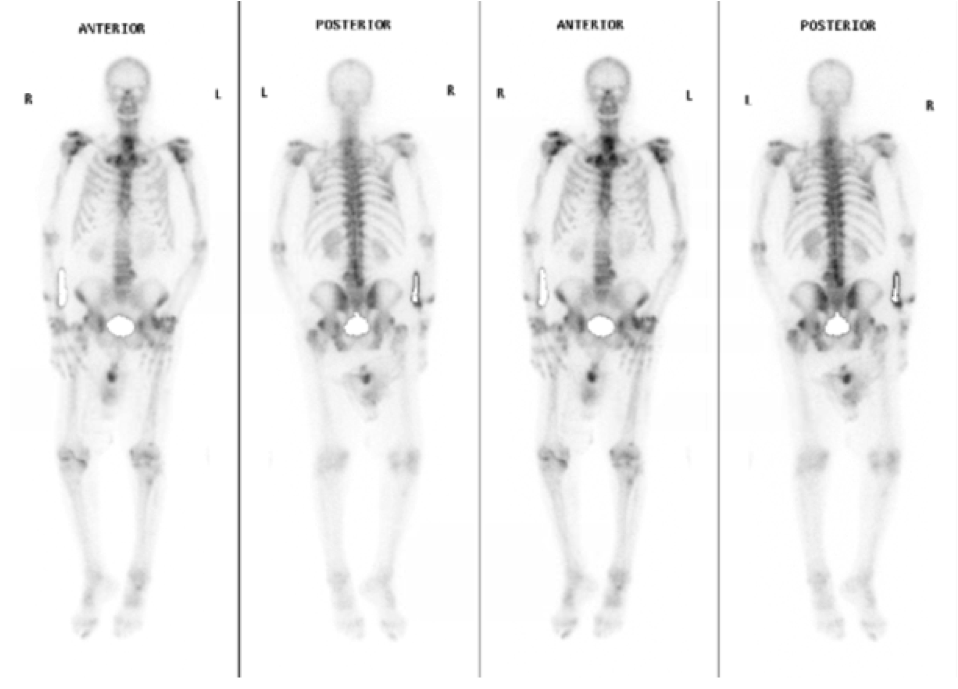
Hospital course: The patient was maintained on voriconazole. Lumbar puncture was performed and was notable for: WBC 4, Glucose 91 (CSF:Serum ratio 0.38) and an elevated protein level of 262. Coccidioides serologies from serum and CSF were obtained, and were both downtrending (Serum 1:32 and CSF 1:16) from previous studies. Imaging demonstrated periosteal reaction with osteopenia and bone mottling, with elevation of alkaline phosphatase.
Question: What is the cause of this patient’s musculoskeletal findings and how would you confirm the diagnosis?
Diagnosis: Voriconazole-induced hyperfluorosis
- Serum Fluoride level was obtained to confirm diagnosis and returned elevated at 15.78 µmol/L (normal < 5)
Discussion:
- Voriconazole is a trifluorinated azole, posing risk of fluoride-induced periostitis with long term use. Our patient had an estimated cumulative dose of 240g; however the cumulative dose does not correlate with risk of periostitis
- Fluoride is absorbed and transferred to bone, creating a crystal structure called fluorapatite. This then stimulates osteoblast activity; however, when fluorapatite integrates into the bone, the bone structure becomes resistant to resorption. This leads to increased bone density, osteosclerosis, bone pain and increased susceptibility to fractures.
- Patients often present with skeletal pain most commonly involving the chest, ribs, arms, forearms and less commonly hips and lower extremities.
- Pain can improve 2-20 weeks after discontinuation of Voriconazole therapy.
- Voriconazole drug levels do not always correlate to patient’s fluoride level, due to differences in fluoride metabolism.
- Diagnosis can be difficult to determine based on imaging alone, bone scans are frequently positive if pain is present and localizes to the described area of pain.
Outcomes:
- Our patient was transitioned to Itraconazole, a nonfluorinated triazole, to continue his life-long therapy for disseminated coccidioidomycosis infection.
- His pain improved over the following 6 months.
- The patient’s laboratory values (alkaline phosphatase and fluoride level normalized over the following 6 months).
References:
- Wermers RA, Cooper K, Razonable RR, et al. Fluoride excess and periostitis in transplant patients receiving long-term voriconazole therapy. Clin Infect Dis. 2011 Mar 1;52(5):604-11.
- Thompson GR, 3rd, Bays D, Cohen SH, et al. Fluoride excess in coccidioidomycosis patients receiving long-term antifungal therapy; an assessment of currently available triazoles. Antimicrob Agents Chemother. 2012;56:563–564.
- Moon WJ, Scheller EL, Suneja A, et al. Plasma fluoride level as predictor of voriconazole-induced periostitis in patients with skeletal pain. Clin. Infect. Dis. 2014; 59(9): 1237-45.
- Skiles JL, Imel EA, Christenson JC, et al. Fluorosis because of prolonged voriconazole therapy in a teenager with acute myelogenous leukemia. J Clin Oncol. 2011;29:e779–782.
