November 2024 Case of the Month
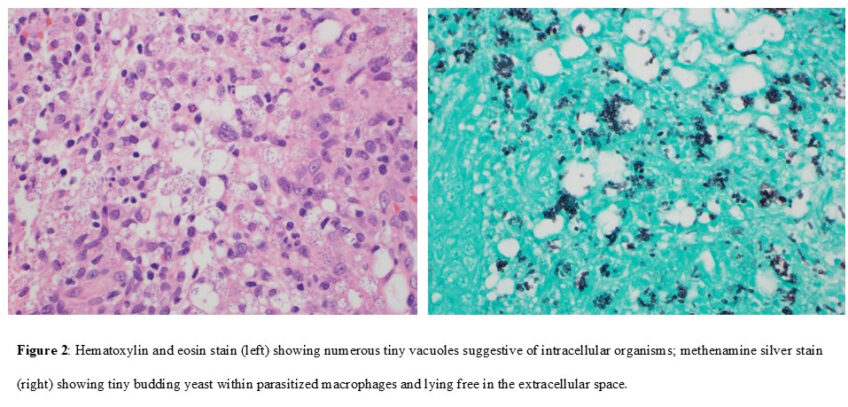
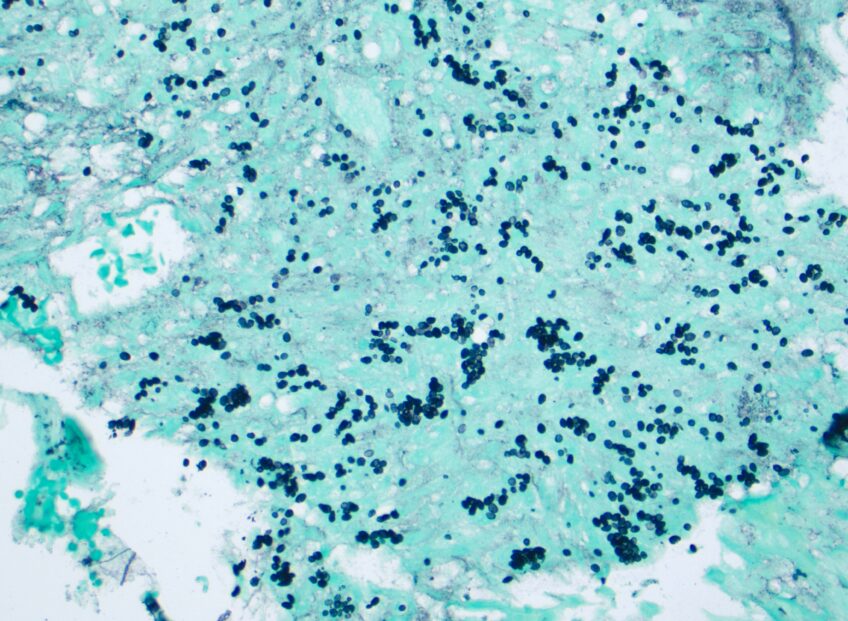
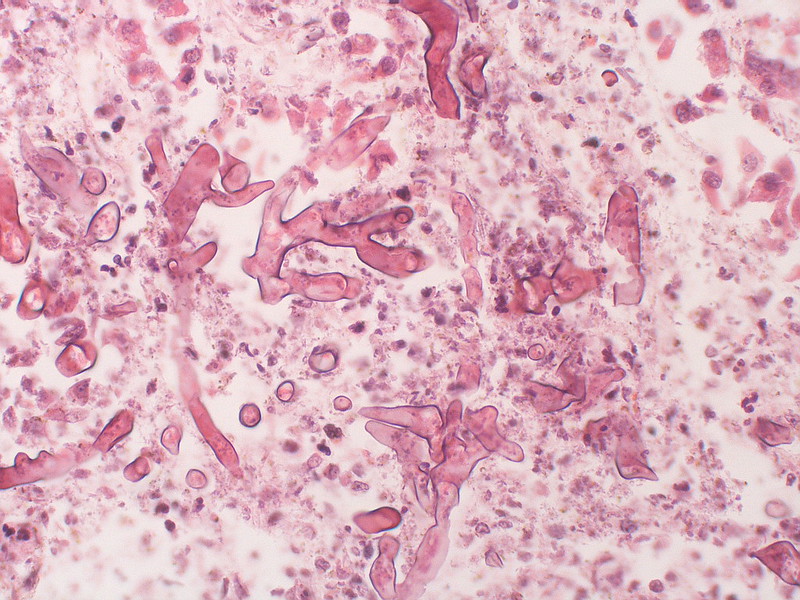
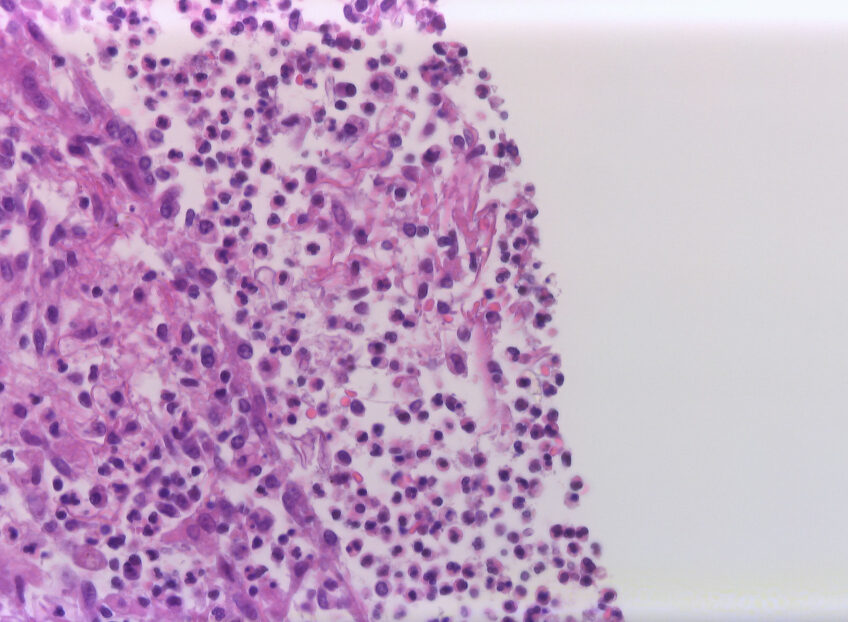
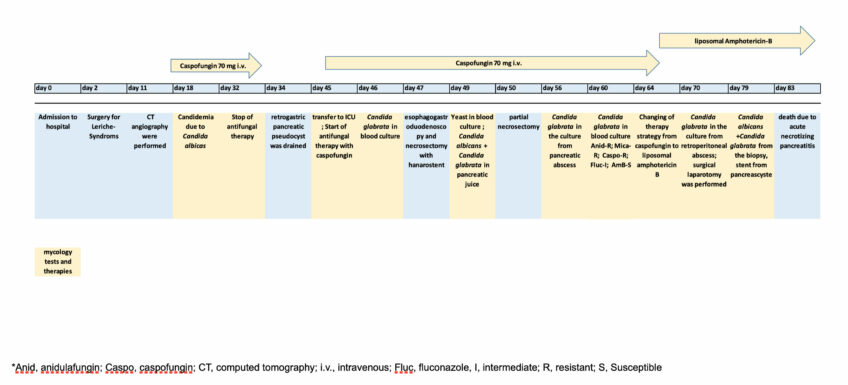
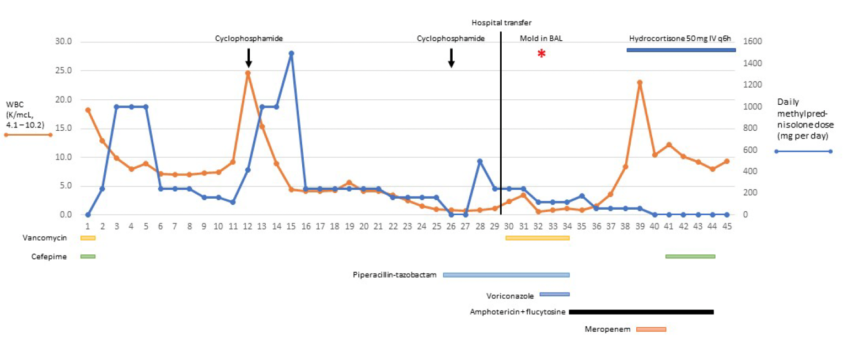
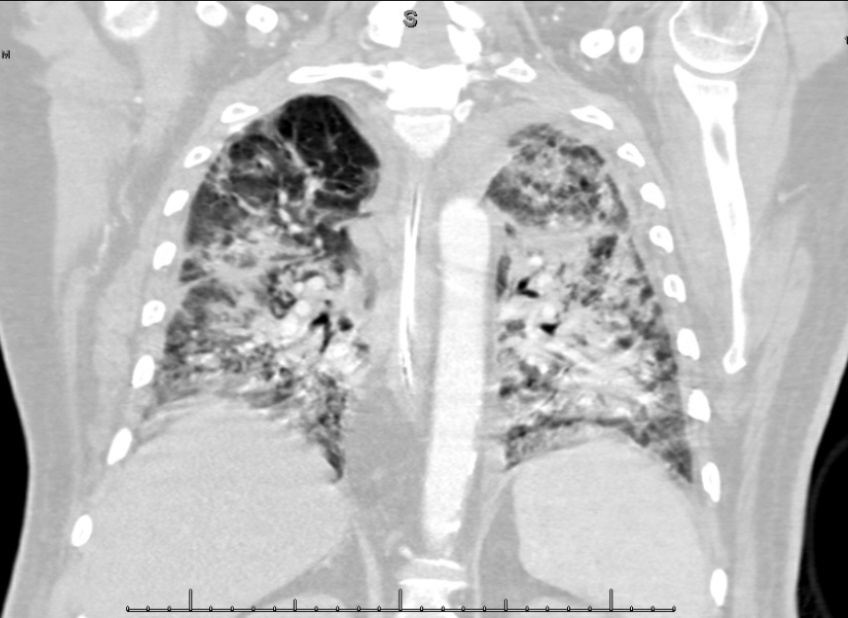
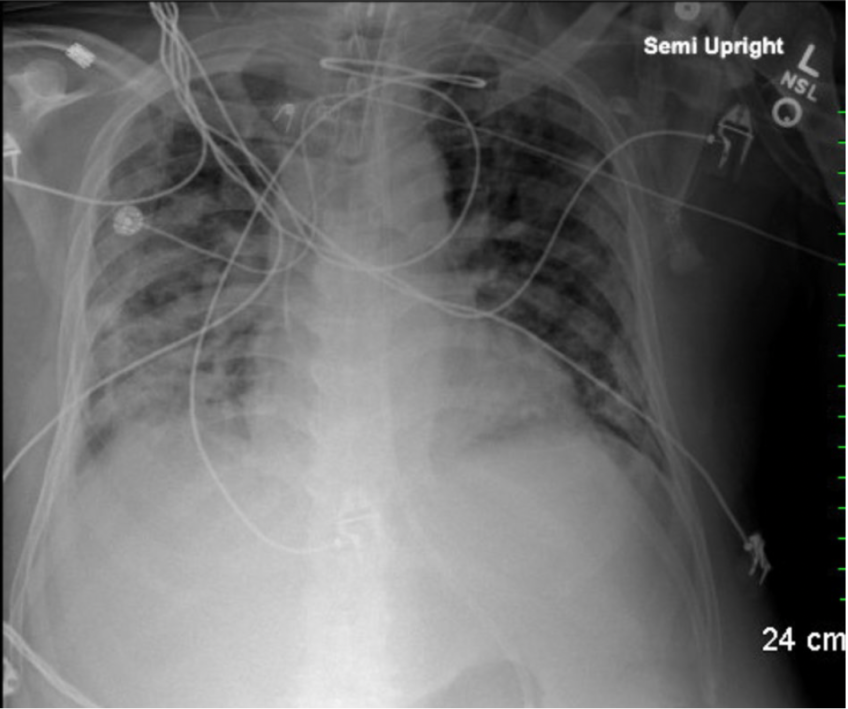
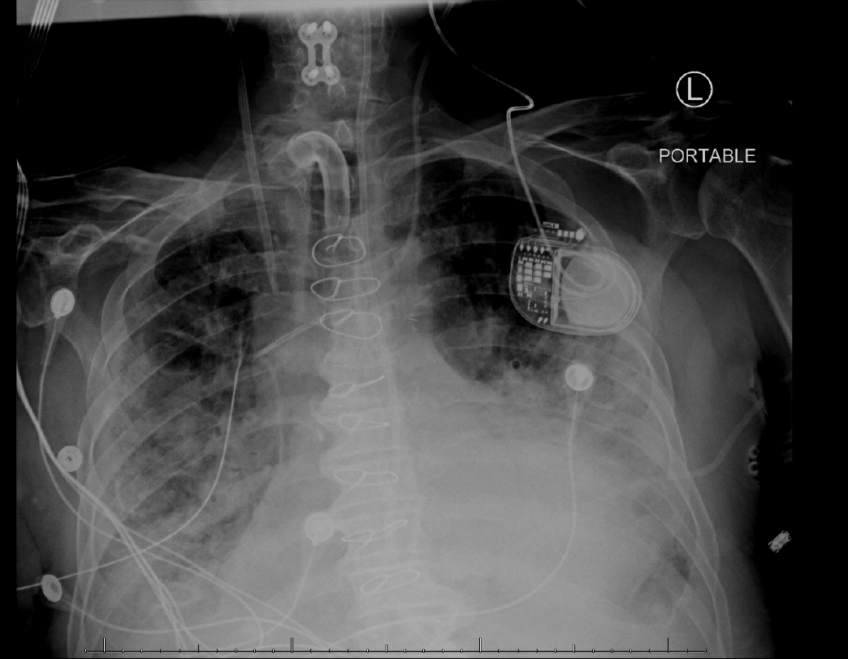
A 23-year-old man, who had received a living related donor renal transplant in 2001 and who was taking mycophenolate mofetil, tacrolimus, and prednisone, underwent facial reconstruction surgery on 12/10/2021 to repair facial fractures sustained in an altercation.