Submitted by: Nico Herrera, MD & Peter Pappas, MD
Institution: UAB
Email: ppappas@uabmc.edu
Date: 02/16/2021
History
Chief Complaint: 78 yo male, COVID+, worsening SOB.
Recent hx: Transferred from OSH for worsening SOB, +CoVID 8 days prior to transfer.
| Medical HX | Social HX | Surgical HX |
| Coronary artery disease | Smoked 50 yrs prior; 1.5-2 ppd x 15 yrs | CABG 10 yrs prior to admission |
| Scalp Melanoma | No illicit drug use, drinks wine socially | Wide local excision (WLE) 4 yrs prior (for scalp melanoma) |
| Depression | Prior engineer, living in central AL | Re-excision and split thickness skin graft 2 yrs prior |
| Hiatal Hernia | Deep brain stimulator in left subthalamic nucleus (STN) 6 months prior | |
| BPH s/p Turp | ||
| Pleural Plaques: Occult aspiration vs asbestosis | ||
| Diverticulosis | ||
| Parkinson’s Disease | ||
| No known allergies |
CT Chest 17 months prior to admission (because of history of melanoma)

-Bilateral calcified pleural plaques are noted without associated effusion
-Subpleural reticulations and patchy ground glass parenchymal opacities especially in the lower lobes and to a lesser degree, right middle lobe and lingual persistent.
Review of Symptoms:
Present
Tachypnea, Shortness of Breath
MEDICATIONS – at admission
Ropinirole 12mg oral daily
Citalopram 20mg daily
Simvastatin 40mg daily
Amantadine 100mg BID
Carbidopa Levodopa 25-100mg 0.5 tabs 4 times daily, 50-200mg nightly
Ubiquinone 600mg AM, 300mg PM
Physical Examination:
Vital signs:
Temp: 96.9 F, HR: 84 bpm, RR: 28 breaths/min, BP: 113/70 mmHg, Weight: 250 lb
General : Alert and in moderate respiratory distress. Skin dry
HEENT: Dry mucous membranes, no pharyngeal erythema
Respiratory: Tachypneic, increased WOB, no wheezing, moving air well
CVS: Difficult to auscultate; NR, RR, no murmurs
GI: Soft, non-tender
Neurology: Oriented, responsive to questions appropriately
Admission Labs:
CHEMISTRY/METABOLIC PANEL
Na – 134 mmol/L
K – 3.9 mmol/L
Cl – 100 mmol/L
HCO3 – 26 mmol/L
BUN – 21 mg/dl
Creatinine – 0.5 mg/dl
Glucose – 116 mg/dl
Ca – 7.6 mg/dl
Total Protein –4.9 gm/dl
Albumin – 2.7 gm/dl
Total Bilirubin – 0.8 mg/dl
AST – 49 units/L
ALT – 14 units/L
ALP – 69 units/L
CBC
WBC – 9.77 x 103/cmm
Hb – 11.4 gm/dl
Platelets – 145 x 103/cmm
%PMNLs – 93
%Lymphocytes – 3
%Eosinophils – 0
Other labs
ABG: pH: 7.39; pCO2: 38.5; pO2: 121; FiO2: 80%
High-sensitive troponin – 2651
Viral Respiratory Panel – Negative
MRSA Nasopharyngeal Screen – Negative
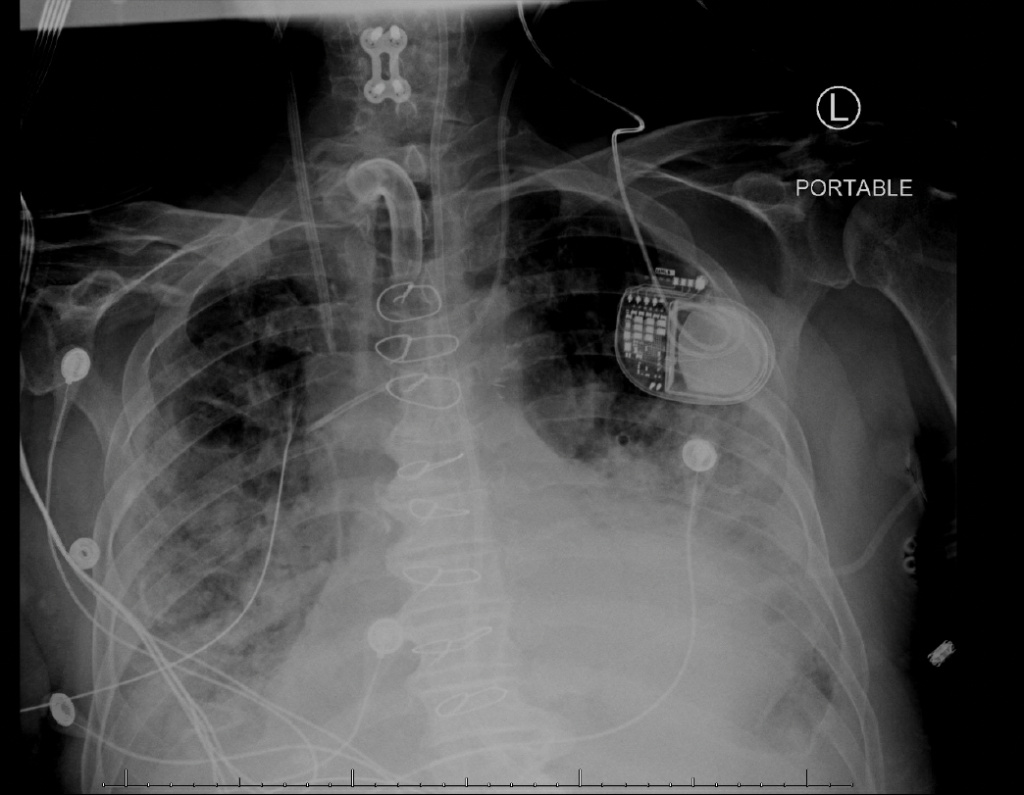
Admission Chest X-Ray
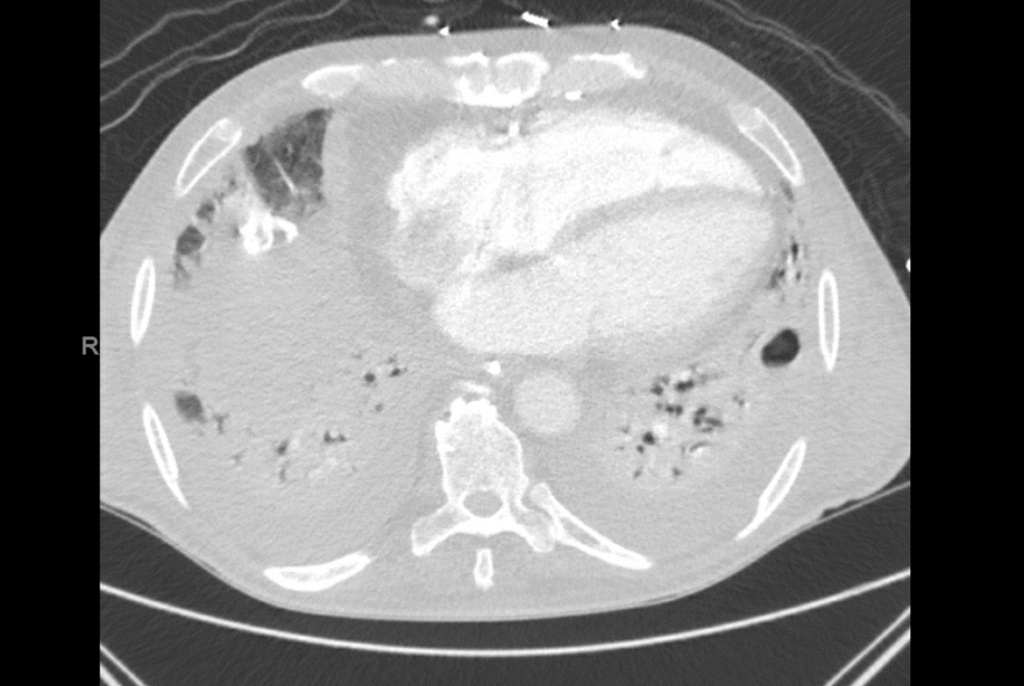
Admission CTA Chest
-Borderline enlarged main pulmonary artery measuring 3.1 cm in diameter.
-Diffuse bilateral ground glass opacities throughout both lungs, most pronounced in the lower lungs. Scattered calcified pleural plaques, unchanged.
-Multiple prominent mediastinal nodes, nonspecific but likely reactive. Stimulator device noted in the anterior upper left chest wall.
-Prominent multilevel bridging, anterior osteophytes of the thoracic spine.
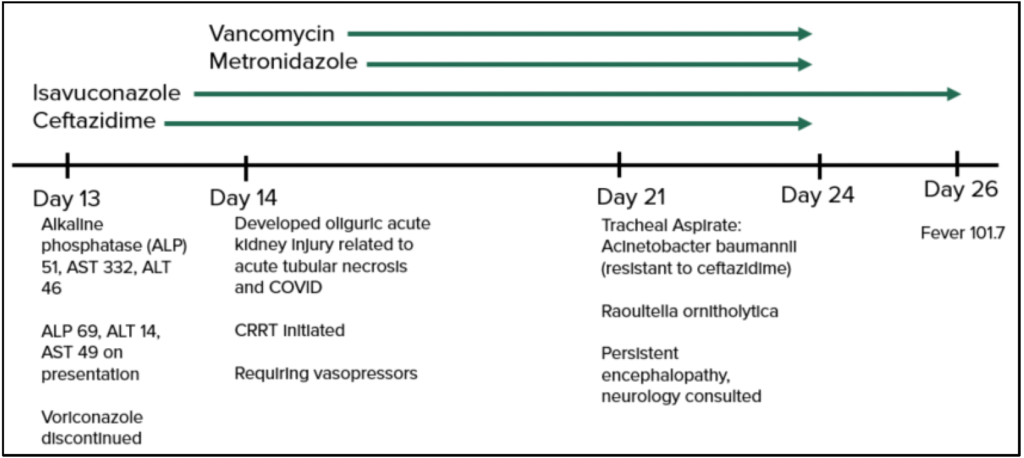
Timeline of Hospital Course / Images
Day 1: Sputum Cultures, imaging
Endotracheal intubation, transferred to MICU
Day 3: Sputum Culture result: Aspergillus fumigatus complex
1-2 Beta D Glucan: < 31
Serum Aspergillus Galactomannan: 2.577
Dexamethasone, Remdesivir, Vancomycin, Cefepime and Azithromycin started
Day 4: Voriconazole started
Day 5: Tracheal Aspirate: Acinetobacter baumannii (ceftazidime sensitive)
Near minimal ventilator settings, failing spontaneous breathing trial
Starts meropenem and minocycline (Day 6-8)
Starts Ceftazidime (Day 9)
Day 10: Tracheal Aspirate: Acinetobacter baumannii; fever 101
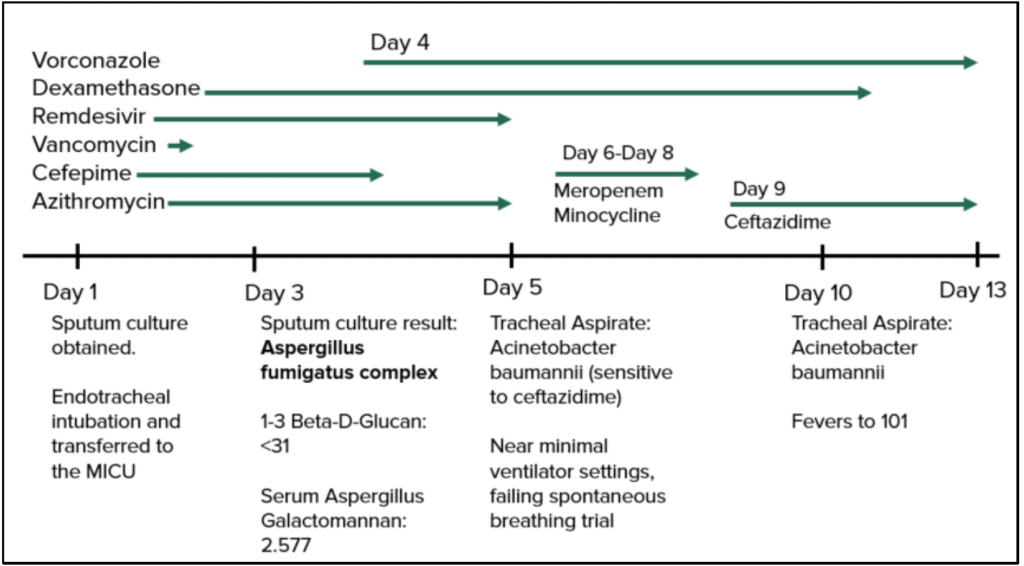
Day 13: Alkaline phosphatase 51, AST 332, ALT 46. Due to elevated AST,
Voriconazole discontinued and Isavuconazole initiated
Day 14: Kidney injury (acute tubular necrosis and COVID)
Requires Vasopressors
Day 21: Tracheal aspirate: A. baumannii (resistant to ceftazidime)
Raoultella ornitholytica
Persistent encephalopathy, Neurology consult
Day 16: Fever 101.7
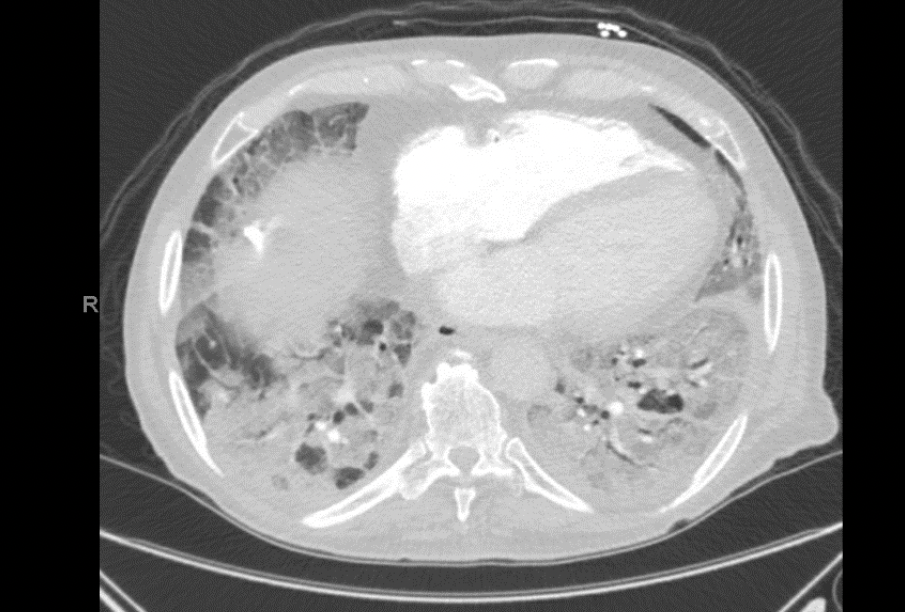
Day 21 – CT Chest
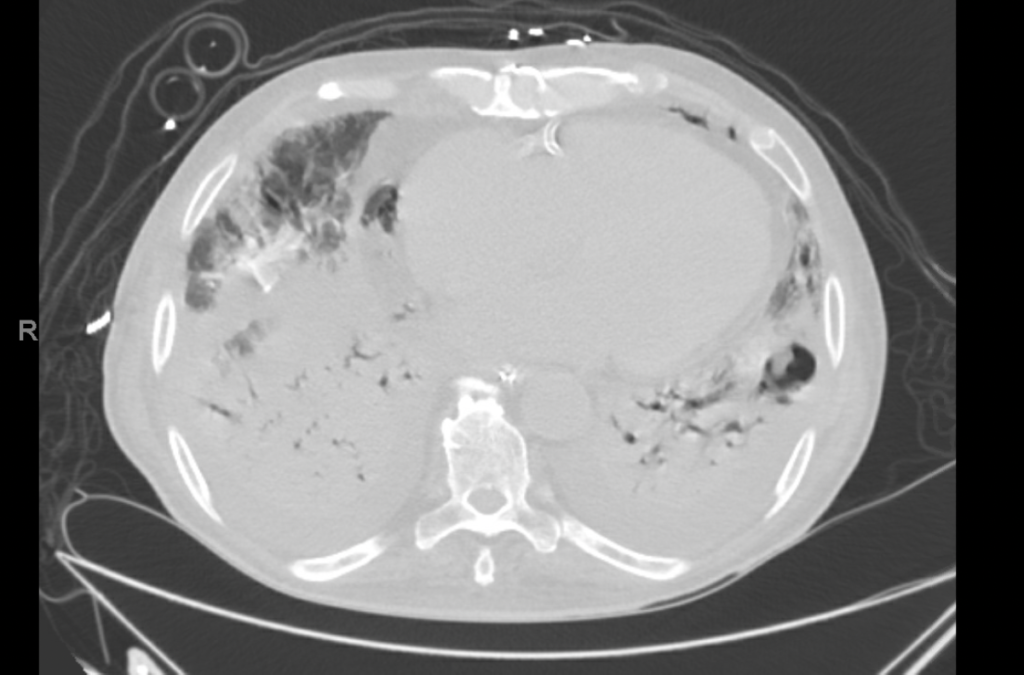
• Small bilateral pleural effusions, right greater than left. Significant improvement and crazy paving pattern of opacities scattered throughout the lungs with interval development of multifocal areas of cavitation in the posterior right upper lobe and left lower lobe. Dense, consolidation in both lower lobes. Small amount of endotracheal and endobronchial secretions present.
• Pneumomediastinum which is new from prior and of uncertain etiology.
• Constellation of findings suggestive of volume overload including small volume ascites and anasarca.
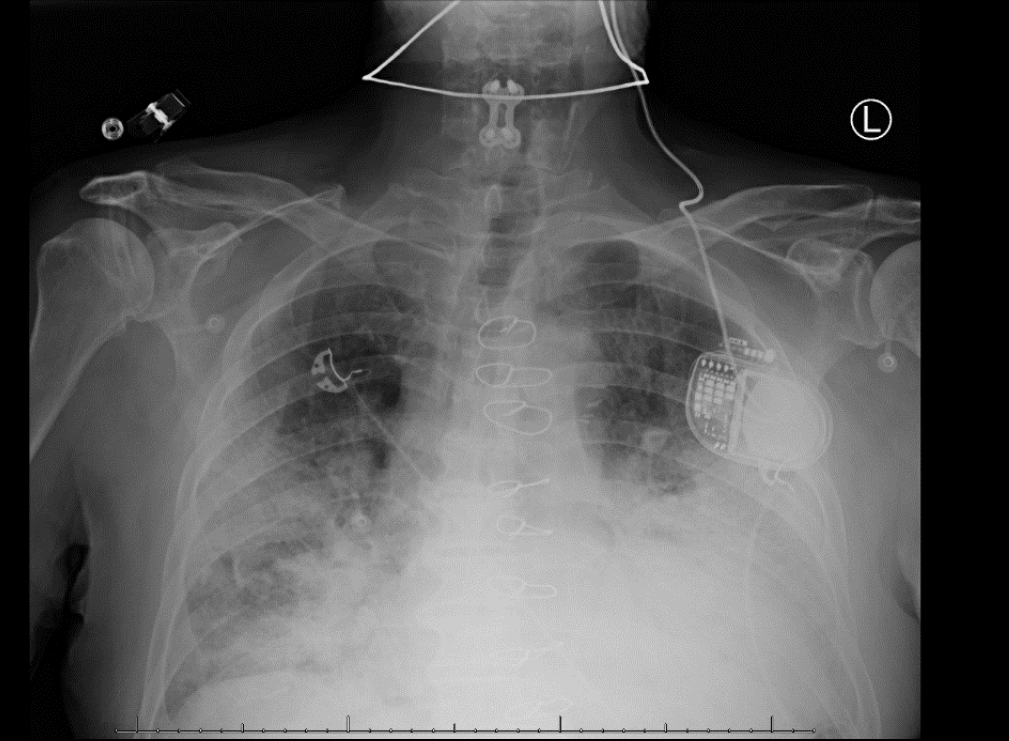
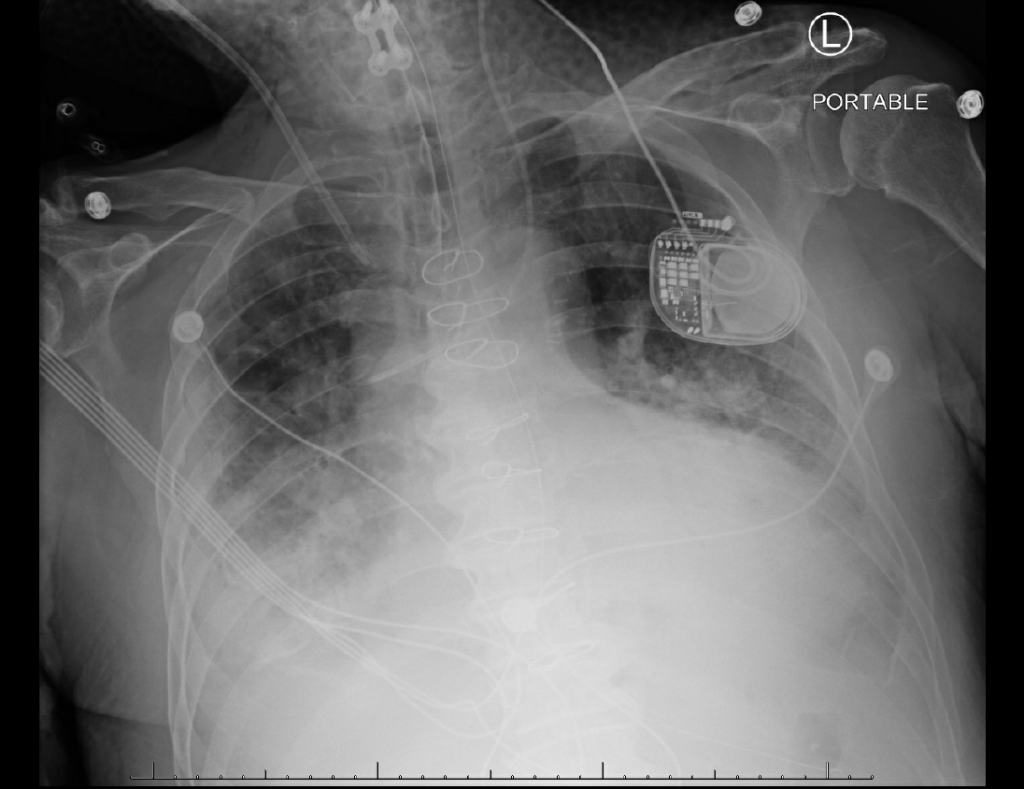
Day 11- Chest Xray
Day 29: Acalculosis cholecystitis; IR guide cholecystostomy
Cultures: C. albicans (fluconazole and micafungin sensitive)
Tracheostomy placed
Day 30: Cardiac Arrest (Pulseless electrical activity (PEA)
Day 35: Transitioned to comfort care
Day 35: Died
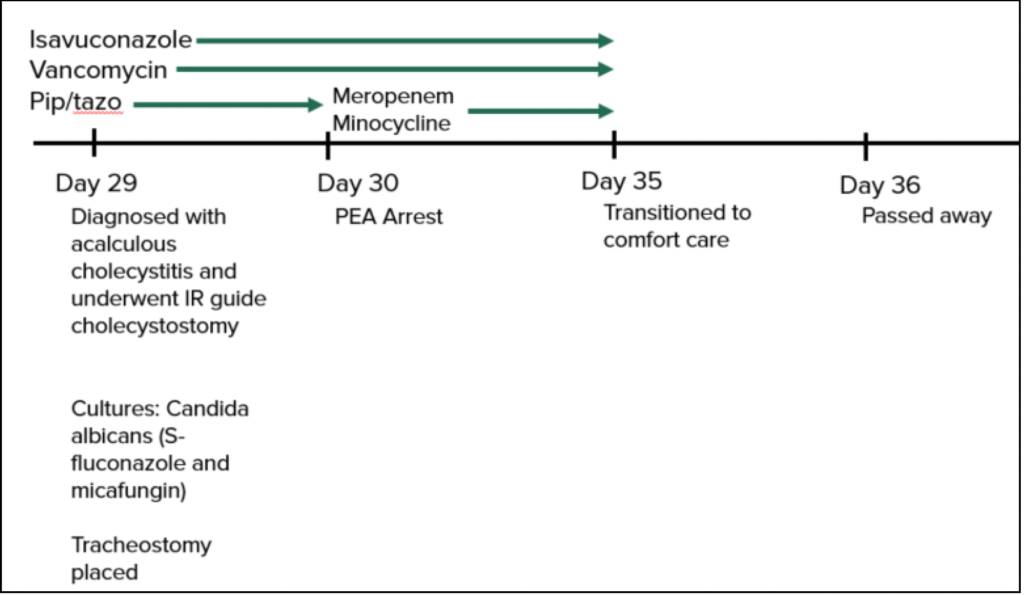
Day 29- Chest CT
• Consolidation in both lower lobes is similar. Patchy peripheral regions of consolidation in the upper lobes represents a worsening. Peripheral cavities near the right lung apex and in the right upper lobe posterior segment appear to be parenchymal and have a similar distribution compared to the previous.
• A few shotty and mildly enlarged mediastinal lymph nodes are slightly larger compared to the previous, possibly reactive.
• Pneumomediastinum is decreased.
• Small bilateral pleural effusions are slightly increase
Day 29- Chest X-Ray