Submitted by: M. Hong Nguyen, MD
Institution: University of Pittsburgh
Email: MHN5@pitt.edu
Date: 6/6/2021
History:
Chief Complaint: fever and shortness of breath
HPI:
56-year-old man was admitted to an outside hospital with fever, short of breath and hypoxia. COVID-19 was diagnosed in the emergency room. He was treated with remdesivir and dexamethasone along with ceftriaxone and azithromycin.
Day 7: He developed acute respiratory distress syndrome requiring intubation. Dexamethasone was continued
Day 9: Due to refractory hypoxemia, he was transferred to our hospital for further management.
Medical Hx
Coronary artery disease with history of cardiac arrest 2016
History of ventricular fibrillation, status post AICD
Hypertension
COPD
Surgical/invasive procedure Hx:
CABG X4 over 10 years ago
Stent placement in 2019
Family Hx
Coronary artery disease and cerebrovascular accident
Social History
Lives in Huntingdon, PA
Tobacco: previous 3 pack per day for 18 years. Quit 2016
Alcohol: Denied
Drugs: Denied
Review of Symptoms:
Unobtainable due to sedation and paralysis
MEDICATIONS – on transfer
Ceftriaxone
Lisinopril
Furosemide
Levothyroxine
Carvedilol
Amiodarone
Apixaban
Physical Examination:
Vital Signs: T 37.5 C, HR 98 bpm, RR 10 breaths/minute, BP 98/42 mmHg
General: Intubated, unresponsive
Cardio: Rate irregularly irregular, no murmur
Pulmonary: Coarse breath sounds throughout. Decreased breath sounds both bases
Abdomen: Bowel sounds present, non-distended, soft
Extremities: 1+ ankle edema
Skin: No rashes
Examination Labs:
CHEMISTRY/METABOLIC PANEL
Creatinine 1.2 mg/dL
AST 27 U/L
ALT 27 U/L
Alk Phos 60 U/L
Total bili 0.6 mg/dL
LDH 753 U/L
CBC
WBC 16.1 x109/L (97% PMN, 1% lymph, 2% mono)
Other labs
Ferritin 753 ng/mL
Lactate 2.6 mmol/L
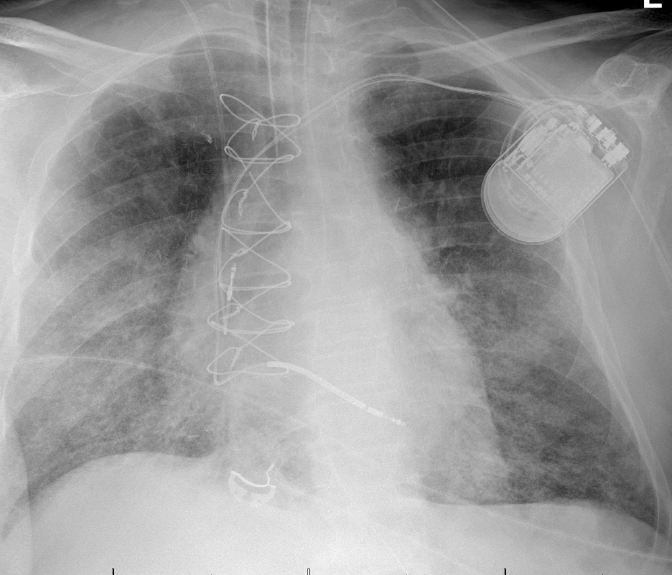
Baseline Chest X Ray (on transfer)
Timeline of Hospital Course:
Day 9 (day of transfer): Bronchoscopy showed friable airways and thick mucus in both lower lobes. He was started on piperacillin-tazobactam. Dexamethasone was stopped
-BAL culture grew 50,000 CFU/mL Chryseobacterium indologenes
Day 10: He was placed on veno-venous extracorporeal membrane oxygenation (ECMO)
Day 12: Leukocytosis resolved (WBC down to 8)
Day 14: Renal function progressively worsened.
Day 17: Creatinine peaked to 4.4 . Urine output was marginal, unresponsive to furosemide
Day 18: Patient was started on continuous renal replacement therapy, but became hypotensive requiring low dose norepinephrine (1 mcg/kg/min) for fluid removal.
Blood and BAL cultures were unrevealing. As per UPMC protocol, surveillance fungal biomarkers with BDG and GM were obtained. BAL culture grew <5.000 CFU/mL Gram negative rods; fungal culture was negative.
BDG = 40 pg/mL
Serum GM = 3.23
BAL GM= 9.04
Day 20: Results of GM prompted CT chest ? cavitary lung lesion RUL. Patient was started on voriconazole and caspofungin. Bronchoscopy did not show a large amount of secretions. BAL fungal culture: no growth
Day 23: Patient suffered two episodes of cardiac arrest. Family decided to make him comfort measure only
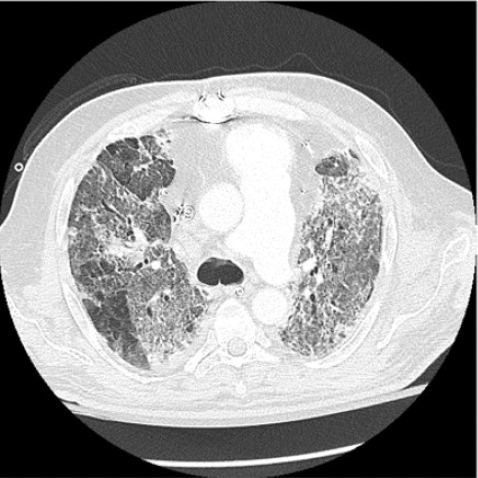
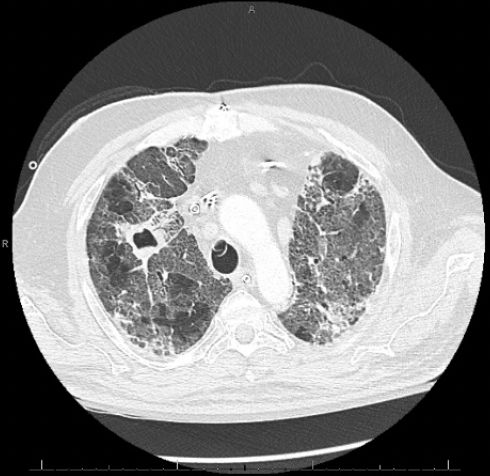
IMAGES (CAT scan of chest Day 18) – diffuse areas of ground glass opacities and traction bronchiectasis involving all lobes, and air bronchograms. There was a 3.3 x 2.7 cm cavitary lesion within the right upper lobe

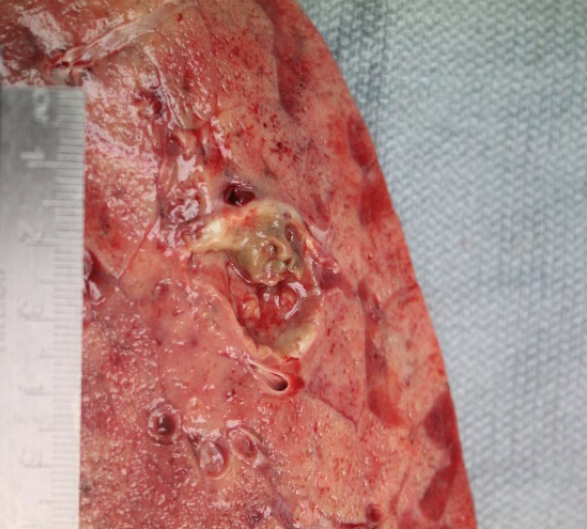
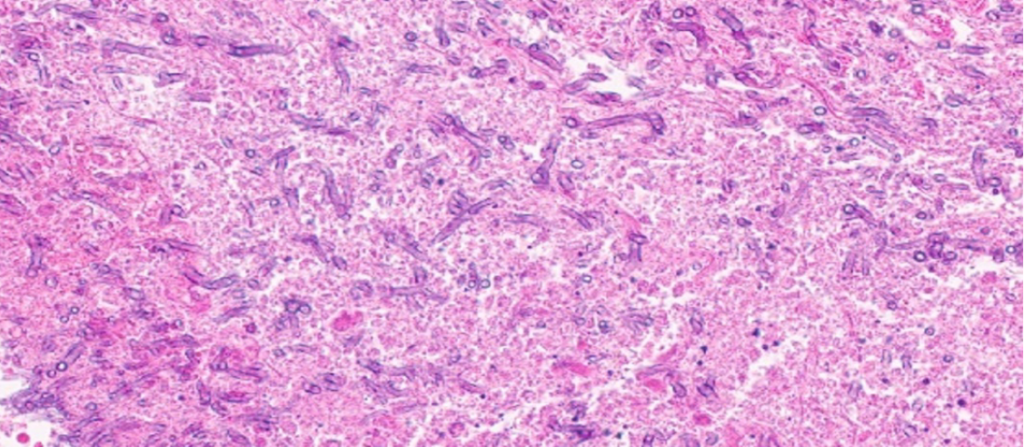
AUTOPSY: The lungs were severely congested with diffuse hemorrphage and parenchymal consolidations. There was a 2.5 x 2.0 x 2.0 cm tan-brown, cavitary lesion in the right upper lobe. Microscopic sections showed extensive invasive branching hyphal structures, acute inflammation, and necrosis.
Go here for continuing education activity and case discussion.
