Submitted by: Edward C Traver, MD and Melanie Malave-Sanchez, MD
Institution: University of Maryland Medical Center
Email: etraver@som.umaryland.edu
Date: 5/27/2021
History:
Chief Complaint: Fatigue
Medical Hx: CAD, MI, CHB s/p pacemaker, pHTN, COPD, DM2, HCV cirrhosis s/p treatment
Family Hx: father (CAD, DM, HTN), mother (CAD, HTN), brother (none), sister (none)
Surgical Hx: pacemaker 3/2019, cervical spine
Review of Symptoms:
Present: fatigue, anorexia, productive cough (w intermittent blood tinge), dyspnea, arthralgias, generalized weakness
Not Present: fever, visual disturbance, chest pain, abdominal pain, back pain, rash, light-headedness, headaches
MEDICATIONS – at transfer: fluticasone-vilanterol inhaler, fluticasone nasal spray, methylprednisolone, montelukast, pantoprazole, piperacillin-tazobactam, pravastatin, umeclidinium, vitamin D
PHYSICAL EXAMINATION: ill and tired appearing, low flow oxygen nasal cannula, bradycardic, diffuse fine crackles throughout the chest, no respiratory distress, left lower extremity pitting edema, strength 4/5 throughout except 3/5 in hip flexors, upper extremity tattoos.
Admission Labs:
CHEMISTRY/METABOLIC PANEL: Creatinine 0.62, Bicarbonate 31, Glucose 47
CBC: WBC 2.3; Hemoglobin 8.3; Platelet 43
Other labs: BAL culture: >10,000 CFU/mL Cryptococcus neoformans; 1,000 CFU/mL Aspergillus fumigatus; <1,000 CFU/mL Normal Upper Respiratory Flora
Timeline of Hospital Course / Images
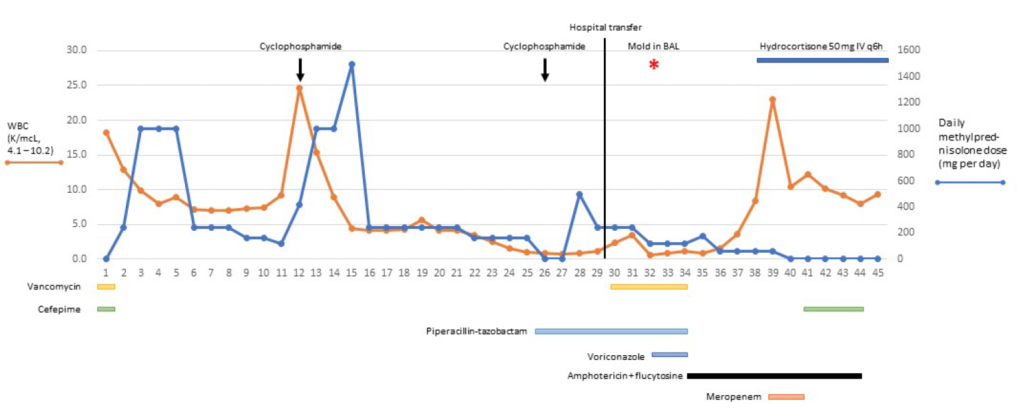
A 59-year-old man was admitted to a different hospital in Maryland, USA in January 2021 with bilateral pneumonia and diagnosed with COVID-19. He was treated with antibiotics, remdesivir, and methylprednisolone. On day 11 he was intubated and 24 hours later given the first of 2 doses of cyclophosphamide for suspected fibrotic lung disease. He was extubated on day 18, but due to persistent hypoxia and progressive pulmonary infiltrates he was transferred to our hospital.
On arrival to our hospital on day 30, he was intubated for the second time and a bronchoscopy was performed. Culture of the bronchoalveolar lavage yielded 2 types of mold on day 32, and MALDI-TOF identified Aspergillus fumigatus and Cryptococcus neoformans. The patient was treated with liposomal amphotericin B and 5-flucytosine for severe pulmonary aspergillosis and cryptococcosis. A lumbar puncture revealed normal opening pressure and cryptococcal antigen was not detected in the cerebral spinal fluid.
On day 39, the patient developed worsening hypoxia and septic shock; sputum culture grew Enterobacter cloacae. Methylprednisolone was changed to hydrocortisone 50 mg IV every 6 hours. On day 43, the patient developed a severe acute kidney injury. Due to the patient’s stated wishes to avoid prolonged mechanical ventilation and renal replacement therapy, his surrogate decision makers withdrew organ support. The patient died on day 45.
WHAT DID YOU FIND MOST CHALLENGING ABOUT THIS CASE?
The patient’s treatment with cyclophosphamide induced severe and lasting immune suppression. Opportunistic infections with fungi may worsen pulmonary function in patients with acute respiratory distress syndrome due to COVID-19. Treatment may be limited by severe toxicity and minimal reserve organ function, as in this patient who additionally developed renal failure on amphotericin and flucytosine.
WHAT DO YOU SEE AS THE GREATEST UNMET EDUCATIONAL NEED IN MANAGING COVID-19–?ASSOCIATED INVASIVE FUNGAL INFECTIONS?
Caution needs to be exercised with use of immunosuppression, especially in the absence of high-quality evidence for its benefit.
Go here for continuing education activity and case discussion.
