Title: COVID-19 and Pulmonary Aspergillus
Submitted by: Elizabeth Thottacherry, Peter Pappas
Institution: UAB
Email: ppappas@uabmc.edu
Date: 2/12/21
HISTORY
Chief Complaint: 63 year old male, presents with shortness of breath and positive SARS-CoV 2 (COVID-19)
Medical Hx Family Hx
Coronary artery disease Father- Renal Cancer
Hypertension Social Hx:
Hyperlipidemia Denies substance abuse, smoking
Asthma Rare alcohol, no history of binge drinking
Chronic back pain
Moderate Obesity (BMI 27 kg/m2
Surgical Hx
Percutaneous coronary intervention
Knee Surgery
REVIEW OF SYMPTOMS:
| Present | Not Present |
| Diaphoresis | Sore Throat |
| Body Aches | Rhinorrhea |
| Insomnia | Diarrhea |
| Chills | |
| Syncope | |
| Dysuria | |
| Headache |
MEDICATIONS – at admission
Aspirin 81mg PO daily
Clopidogrel 75mg PO daily
Dexlansopraxole 30 mg PO daily
Lisinopril/Hycrochlorothiazide 10mg/12.5 mg PO daily
Meloxicam 7.5mg PO daily
Clonazepam 1mg PO BID, as needed
PHYSICAL EXAMINATION:
Vital signs:
Temp: 99.8 F/37.7 C, HR: 81 bpm, RR: 20 breaths/min, BP: 146/81 mmHg, Weight: 250lb
General : Alert and oriented in no distress
HEENT: Normocephalic, supple neck, trachea midline, extraocular movements intact, moist oral mucosa
Respiratory: Clear bilaterally, tachypneic
CVS: S1, S2, RRR, no murmurs
GI: Soft, non-distended, BS +
Neurology: Oriented, no focal deficits
ADMISSION LABS
CHEMISTRY/METABOLIC PANEL
Na – 127 mmol/L
K – 3.9 mmol/L
Cl – 92 mmol/L
HCO3 – 26 mmol/L
BUN – 17 mg/dl
Creatinine – 0.9 mg/dl
Glucose – 110 mg/dl
Ca – 9.0 mg/dl
Total Protein –7.1 gm/dl
Albumin –
Total Bilirubin – 0.9 mg/dl
AST – 144 units/L
ALT – 220 units/L
ALP – 125 units/L
CBC
WBC – 8.38 x 103/cmm
Hb – 15.1 gm/dl
HCT – 45%
Platelets – 210 x 103/cmm
%PMNLs – 79
%Lymphocytes – 13
%Eosinophils – 0
Other labs
LDH – 586 units/L (120 – 240 units/L)
Troponin – 6 ng/L (3 – 20 ng/L)
Ferritin – 2029 ng/ml (23.9 – 226.2 ng/ml)
ESR – 60 mmg/hr (0 – 10 mm/hr)
D dimer – 372 ng/ml (0 – 240 ng/ml)
ESR – 752 mg/dl (220 – 498 mg/dl)
Urinalysis – unremarkable
SARS CoV 2 RT-PCR – DETECTED
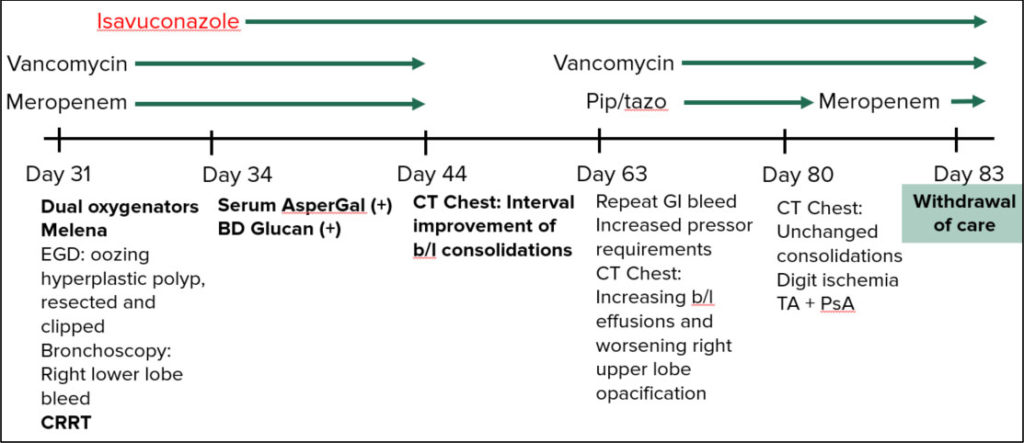
TIMELINE OF HOSPITAL COURSE/IMAGES
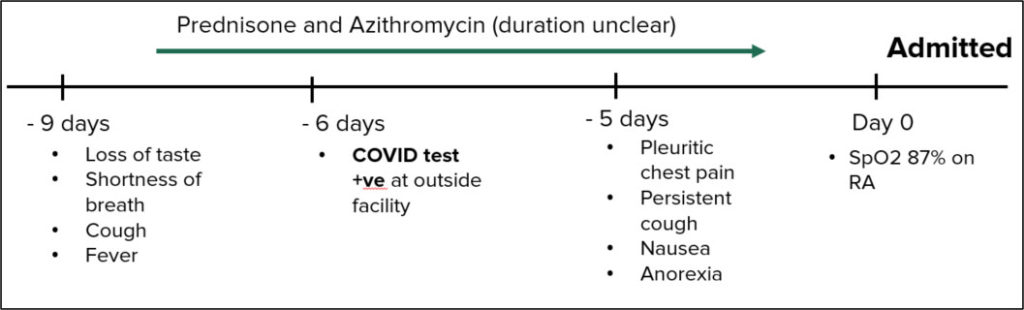
COVID 19 Diagnosis/Timeline:
Day -9: Shortness of breath, fever, loss of taste
Day -6: COVID Test positive at outside facility
(Prednisone and Azithromycin- duration unclear
Day -5: pleuritic chest pain, persistent cough, nausea, anorexia
Day 0: Sp02 87% on room air, put on nasal cannula 2L 02 advanced to 6L 02
Medications Added: Dexamethasone, Remdesivir, Anakinra
Cultures: Blood cultures – negative
Antigens: Legionella Urine Ag negative
Day 0 – Admission Chest Xray

Day 2: HFNC 50L/100%, BIPAP QHS; Transferred to ICU; iEPO
Day 7: Endotracheal intubation; Prone ventilation
Trans Thoracic Echo (TTE): EF 55% – 60%; Doppler US: no lower limb DVTs
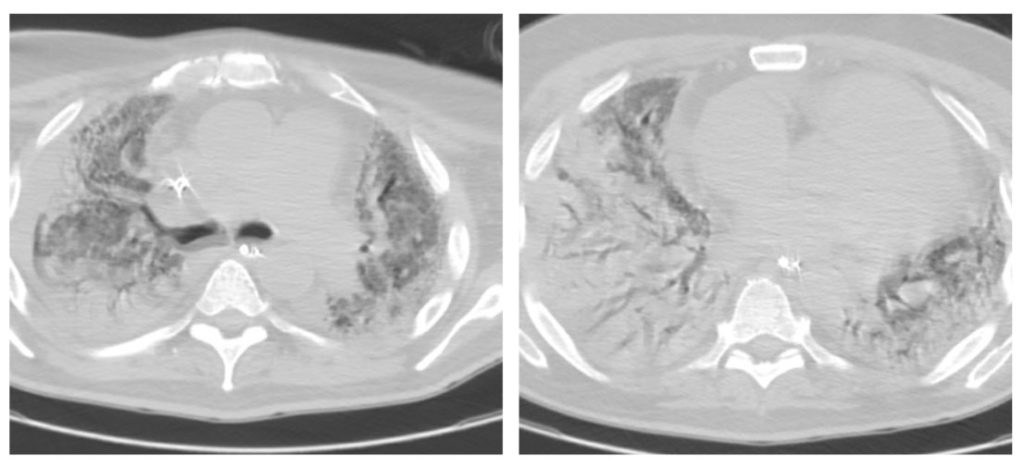
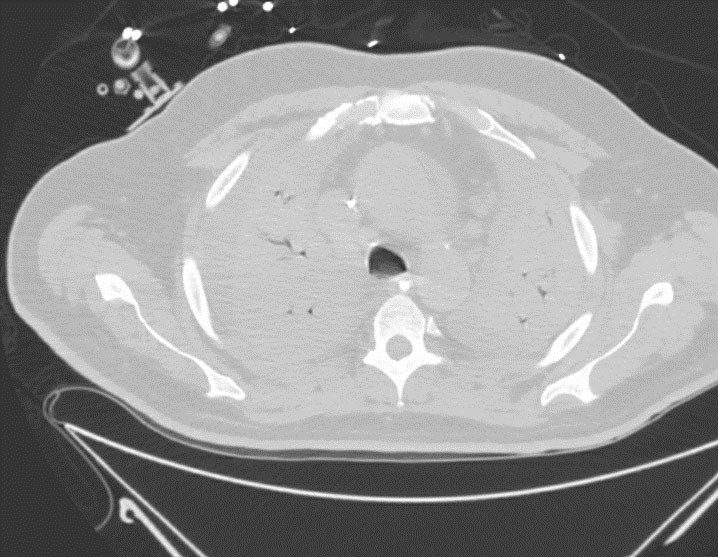
CTA Chest: B/L extensive ground glass opacities and confluent consolidation,
No PE.
Medication Added: Vancomycin, Cefepime
Cultures: Blood cultures – 2/4 bottles S. epidermidis
T2 Candida – negative
Tracheal Aspirate- Negative
Day 7: CTA Chest w/ and w/o contrast


Day 10: Blood Cultures – negative; T2 Candida- Negative
Day 11: Cannulated for VV ECMO; CT Head: B/L SAH; Bronchoscopy
Cultures: BAL- CMV, HSV, Legionellaa, Fungal and Bacterial cultures all negative
BAL HSV PCR negative; Viral respiratory panel Negative; AsperGal- negative; Beta D glucan- negative
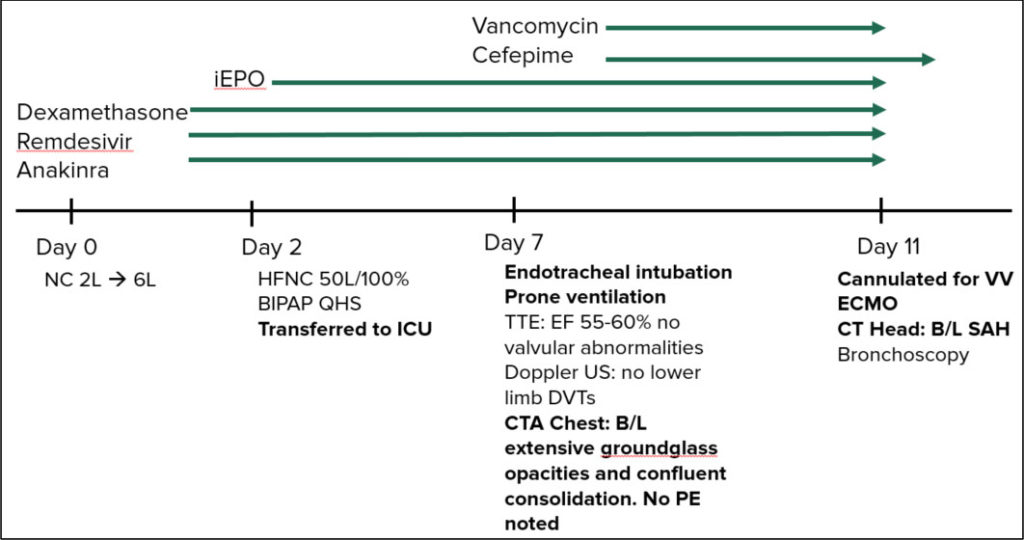
Day 19: Tracheostomy/PEG; Dual oxygenators; Melena
EGD: oozing hyperplastic polyp, resected and clipped
Bronchoscopy: RLL bleed; CRRT (Continuous renal replacement therapy)
Cefepime, Vancomycin continued
Day 20: COVID-19 IgG – positive
Day 24: P/F ratio: 99 (normal is >400); NO started
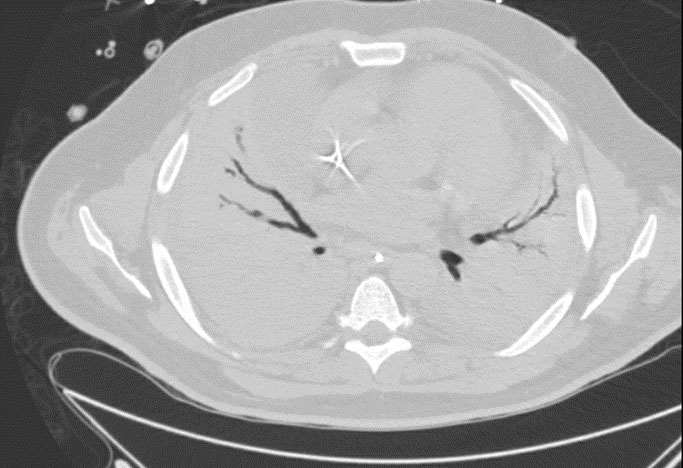
CT Chest: Diffuse bilateral consolidation with moderate bilateral pleural effusions
CT Abdomen/pelvis: no abnormalities
Added Pip/tazo
Day 22, 26, 29- BAL Legionella, Fungal and bacterial culture negative
Day 28: Cardioversion for atrial fibrillation; TTE: Dilated RV, EF 55-60%
Medications added: Norepinephrine, Vasopression, Epinephrine, Amiodarone, Meropenem and Vancomycin continues
Day 31: Lactic acidosis, increased vasopressor requirements; Leukocytosis.
ID CONSULT
Blood culture and T2 Candida negative
Dual Oxygenators
Melena; EGD: oozing hyperplastic polyp, resected and clipped
Bronchoscopy: RLL Bleed; CRRT
Day 24- Chest CT w/o contrast
Day 32: Isavuconazole started
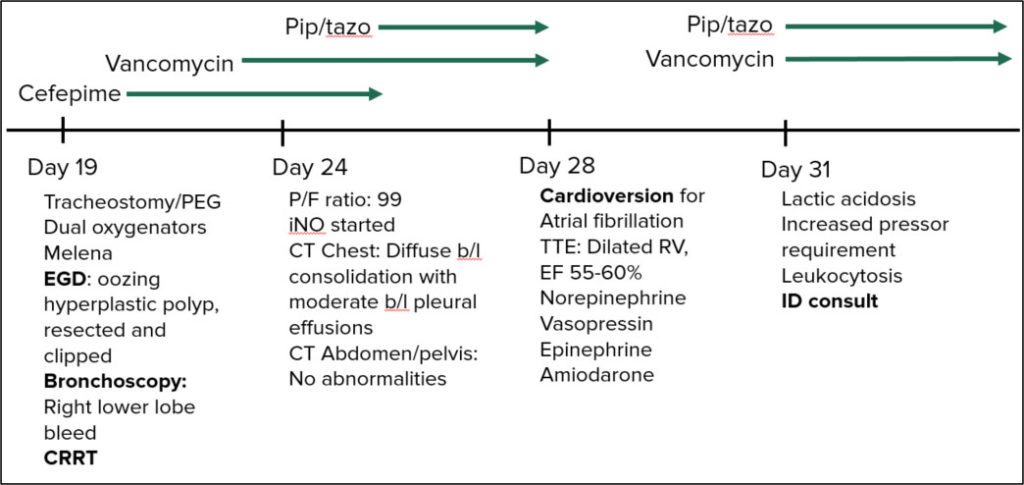
Day 34: Serum AsperGal – positive; BD Glucan – positive
Isavuconazole continued
Day 44: CT Chest- interval improvement of bilateral consolidations
Day 63: Repeat GI Bleed, increased vasopressor requirements
CT Chest- Increasing bilateral effusions and worsening right upper lobe opacification
Day 80: CT Chest: unchanged consolidations, Digital ischemia; TA + PsA
Day 83: Withdrawal of care, deceased.
Day 44- CT Chest w/o contrast – patchy consolidation in both lungs with areas of dense infiltrates
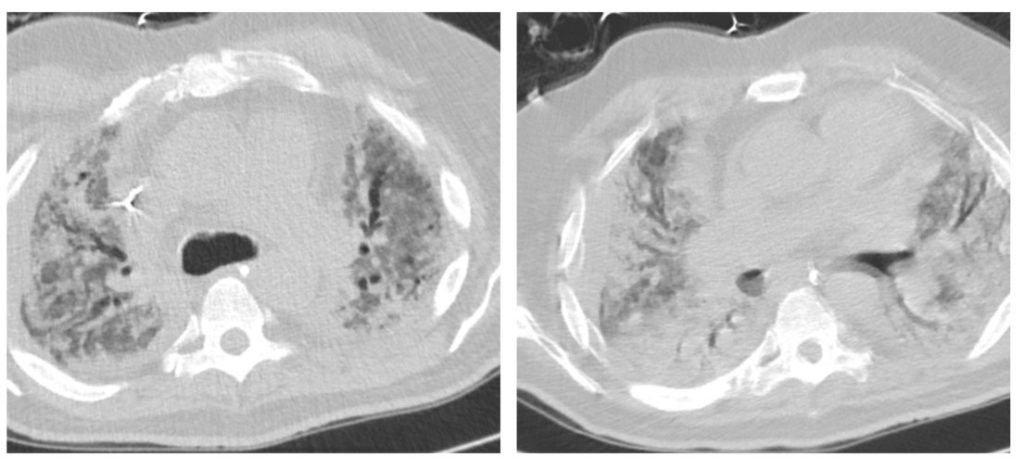
Day 80- CT Chest w/o contrast – Progressive dense, bilateral consolidation throughout both lungs