Title: Botryosphaeriaceae spp. Tenosynovitis in an Immunocompetent Patient
Submitted by: James Dickey MD, Caroline Hamilton PA-C, MPH, Hasan Samra MD, Jose Vazquez MD
Institution: Medical College of Georgia at Augusta University
Email: jadickey@augusta.edu
Date Submitted: 1/4/2023
History:
A 58-year-old male presented to our health system’s walk-in orthopedic clinic complaining of worsening pain and swelling of the third 3rd digit of his left hand. He reported that three weeks prior to presentation, he was trimming bushes in his yard when he was stuck by a thorn into the proximal phalanx of the 3rd digit. He had severe swelling and pain over the volar aspect of the phalanx that acutely worsened after five days. The patient initially presented to his primary care provider for treatment. He was prescribed sulfamethoxazole-trimethoprim, of which he had completed seven days of treatment on presentation to the orthopedic clinic. He reported improvement of swelling but persistent pain and stiffness of the finger since initiation of antibiotics.
Physical Examination:
On physical examination, he was afebrile and in no acute distress. The patient was holding the left 3rd digit in slight flexion. There was volar swelling with minor erythema of the entire length of the proximal phalange of the left digit. There was tenderness over the proximal phalanx, first annular pulley, and the distal phalanx up to the distal end of the flexor sheath of the digit. The patient had pain with passive extension and attempted flexion. He was able to fire the flexor digitorum profundus and flexor digitorum superficialis. There was no fusiform swelling. The contralateral extremity was normal.
Laboratory Examination:
No laboratory tests were ordered on initial evaluation.
Radiology:
X-ray of the left hand was without abnormal findings.
History (cont.):
Based on the clinical history and physical exam findings, the patient was diagnosed with flexor tenosynovitis. Due to disease progression and lack of improvement on oral antibiotics, the following day the patient underwent left long finger incision and drainage with irrigation of flexor sheath and left flexor digitorum profundus partial debridement and synovectomy.
On incision into the digit, synovitis was evident throughout the tendons and pulley region, extending from the first to the fourth annular pulley. There was a small area of purulence that was sent for bacterial and fungal culture. There was significant degeneration of the 3rd annular pulley, which was excised and sent for additional culture. At the flexor digitorum profundus tendon, there was an area of degeneration and a small tip of what appeared to be the retained thorn.
Question 1: What are probable/possible diagnoses?
Based on the intraoperative findings, the surgical team became concerned for bacterial and or fungal infection. The infectious disease team was consulted. A fungal etiology was thought to be unlikely, and the patient was empirically initiated on doxycycline 100mg twice a day for ten days.
Microbiology/Diagnostic Tests Performed:
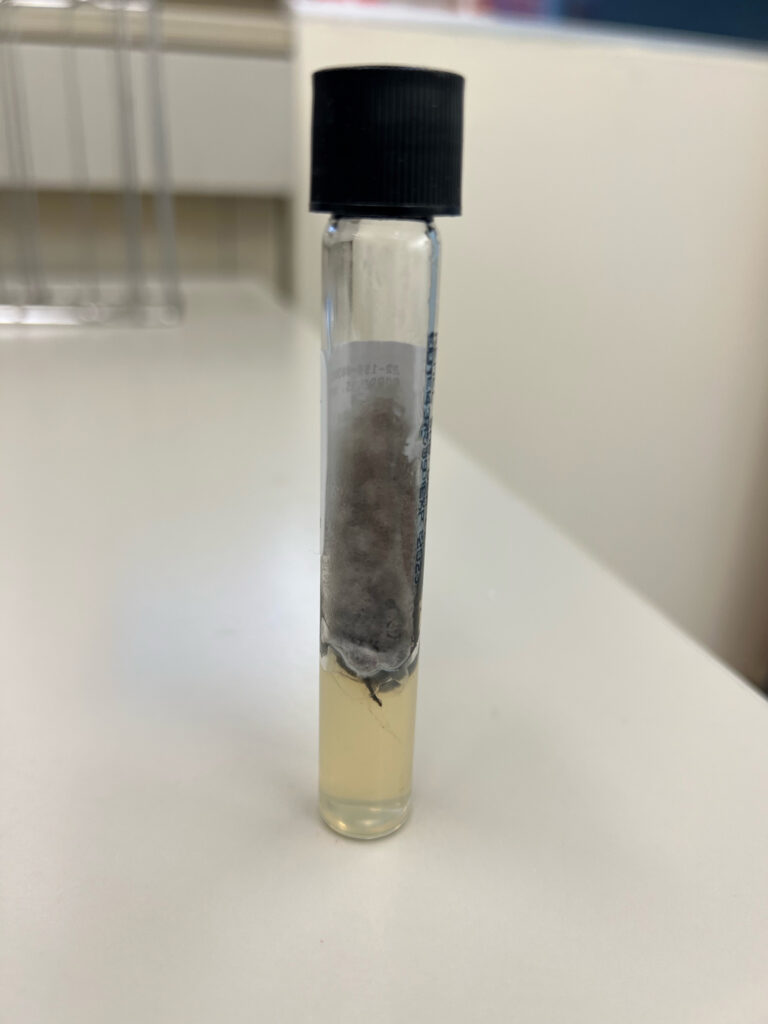
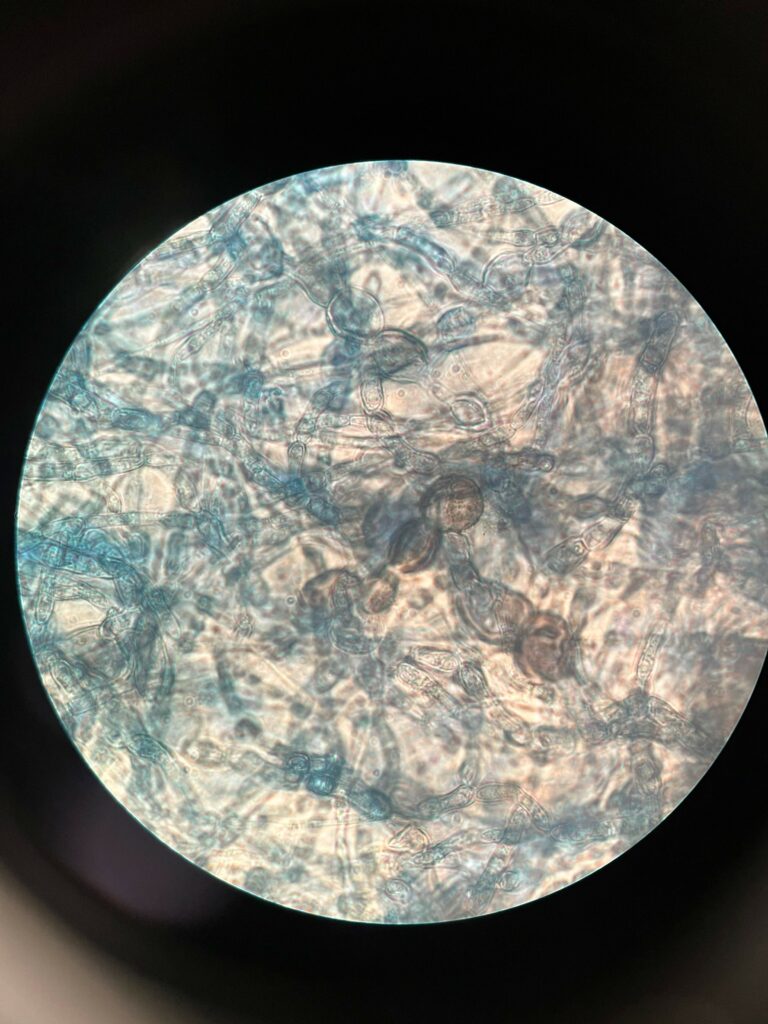
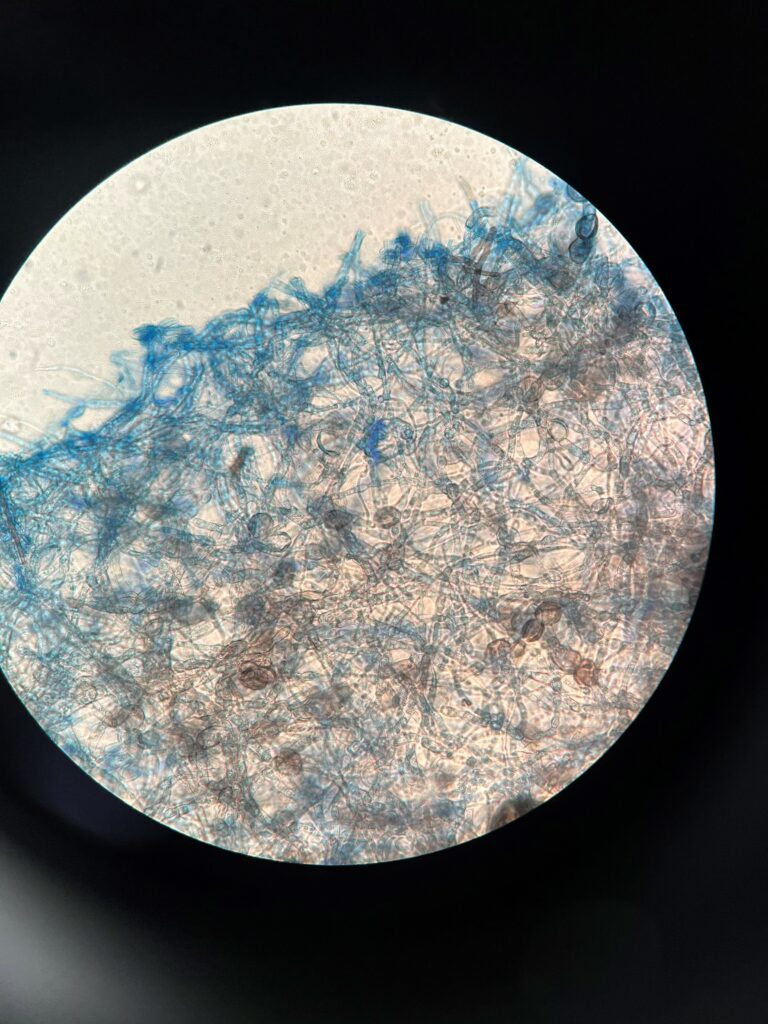
The bacterial cultures finalized with no growth. The fungal tissue culture grew a mold 5 weeks post operation. The isolated mold showed gray black, dry, slightly raised colonies (Figure 1). Lactophenol cotton blue stain (Figure 2) showed dark (melanin) arthroconidia, brown-colored hyphae and lemon-shaped ascospores. The microbiology lab was unable to identify the mold based on macroscopic and microscopic features. The isolate was sent to a reference laboratory for DNA sequencing and identified as a Botryosphaeriaceae species. Identification was complete approximately seven weeks after surgery.
Final Diagnosis: Botryosphaeriaceae spp. tenosynovitis of the left 3rd digit.
Question 2: What treatment is recommended in the care of this patient?
Treatment: PO voriconazole 200mg twice daily
Outcome: After identification of the mold nearly two months after surgical washout, the patient was started on voriconazole 200mg twice daily which he took for 4 weeks. At the three month post-operative follow up appointment, he had regained near full range of motion of the left 3rd digit with no pain or swelling.
Discussion: (500 words)
Phaeohyphomycosis is an infection caused by dematiaceous, or melanized, fungi. It refers to a broad spectrum of infections, ranging from localized superficial and subcutaneous infections to disseminated and/or invasive infections causing end organ damage.
Botryosphaeriaceae are a family of endophytic fungi found in woody plants in tropical and subtropical environments globally. The genera comprising this family include numerous plant pathogens that hold major significance in agriculture and forestry causing branch dieback, fruit rot, and plant death [1]. Human infection by these fungi is very rare. The most commonly reported Botryosphaeriaceae spp. causing human disease are the dematiaceous Neoscytalidium spp. (formerly Scytalidium) and Nattrassia mangiferae (formerly Hendersonula toruloidea). Onychomycosis and superficial skin infections are the most common forms of infection [2, 3]. Cases of disseminated or invasive infection are even less common and tend to occur in immunocompromised individuals. Reports of these infections include subcutaneous infection, sinusitis, myecetoma, and central nervous system abscesses. Notably, several of these cases have been reported in solid organ transplant recipients [2, 4-10].
Among reports of Botryosphaeriaceae spp. phaeohyphomycosis, only two cases have been reported in immunocompetent individuals in the absence of trauma. These include a case of cerebral abscess and a case of pleural infection by Neoscytalidium dimidiatum [11, 12].
There are three reported cases of infection involving the eye or orbit resulting in endophthalmitis or keratitis in immunocompetent individuals. Moreover, there is an additional case of fatal orbital gas gangrene in a cirrhotic and diabetic individual. Interestingly, in all four cases, patients reported trauma of a thorn or plant-like material to the eye or orbit that likely resulted in traumatic implantation of Botryosphaeriaceae spp. [13-16].
In contrast , this patient was immunocompetent with no significant past medical history. His reported history of a thorn puncture wound combined with the intraoperative findings and a positive culture is consistent with prior cases of traumatic implantation of Botryosphaeriaceae spp. However, this appears to be the first case of a penetrating injury into synovial tissue, producing a significant tenosynovitis infection in an immunocompetent host.
As invasive Botryosphaeriaceae spp. phaeohyphomycosis is exceedingly rare, there are no definitive treatment guidelines for therapy. Successful treatments have included amphotericin B, voriconazole, and posaconazole [17].
The initial choice to empirically treat with doxycyline following operative debridement was reasonable in this case. A recent, limited study examining the causative organisms of thorn-associated infections in Arizona found that typical cutaneous organisms, such as Stapylococcus spp., caused the majority of these infections. Of the 58 culture-proven infections examined, fungi were identified in only four total cultures. These organisms were limited to Aspergillous spp., Candida spp., and Paecilomyces lilacinus.
This unique case demonstrates the importance of retaining a high clinical suspicion for atypical pathogens following antibiotic treatment failure even among immunocompetent individuals. In individuals reporting a penetrating injury, clinicians should consider the increased risk of traumatic implantation of environmental fungal pathogens, as exemplified in the case presented here.
Key References:
1. Slippers, B. and M.J. Wingfield, Botryosphaeriaceae as endophytes and latent pathogens of woody plants: diversity, ecology and impact. Fungal biology reviews, 2007. 21(2-3): p. 90-106.
2. Garinet, S., et al., Invasive cutaneous Neoscytalidium infections in renal transplant recipients: a series of five cases. BMC Infect Dis, 2015. 15: p. 535.
3. Ungpakorn, R., Mycoses in Thailand: current concerns. Nihon Ishinkin Gakkai Zasshi, 2005. 46(2): p. 81-6.
4. Tan, D.H., et al., Disseminated fungal infection in a renal transplant recipient involving Macrophomina phaseolina and Scytalidium dimidiatum: case report and review of taxonomic changes among medically important members of the Botryosphaeriaceae. Med Mycol, 2008. 46(3): p. 285-92.
5. Willinger, B., et al., Disseminated infection with Nattrassia mangiferae in an immunosuppressed patient. Journal of clinical microbiology, 2004. 42(1): p. 478-480.
6. Geramishoar, M., et al., First case of cerebral phaeohyphomycosis caused by Nattrassia mangiferae in Iran. Jpn J Infect Dis, 2004. 57(6): p. 285-6.
7. Zaatari, G.S., R. Reed, and R. Morewessel, Subcutaneous Hyphomycosis Caused by Scytalidium hyalinum. American Journal of Clinical Pathology, 1984. 82(2): p. 252-256.
8. Sigler, L., et al., Invasive Nattrassia mangiferae infections: case report, literature review, and therapeutic and taxonomic appraisal. Journal of Clinical Microbiology, 1997. 35(2): p. 433-440.
9. Dunn, J.J., et al., Invasive fungal sinusitis caused by Scytalidium dimidiatum in a lung transplant recipient. Journal of clinical microbiology, 2003. 41(12): p. 5817-5819.
10. Benne, C.A., et al., Disseminating infection withScytalidium dimidiatum in a granulocytopenic child. European Journal of Clinical Microbiology and Infectious Diseases, 1993. 12(2): p. 118-121.
11. Mani, R.S., et al., Cerebral phaeohyphomycosis caused by Scytalidium dimidiatum: a case report from India. Med Mycol, 2008. 46(7): p. 705-11.
12. Elinav, H., et al., Invasive Scytalidium dimidiatum infection in an immunocompetent adult. Journal of clinical microbiology, 2009. 47(4): p. 1259-1263.
13. Al-Rajhi, A.A., et al., Scytalidium dimidiatum fungal endophthalmitis. The British Journal of Ophthalmology, 1993. 77(6): p. 388.
14. Gumbo, T., et al., Case report. Nattrassia mangiferae endophthalmitis. Mycoses, 2002. 45(3?4): p. 118-119.
15. Ruban, V.V., et al., Keratitis due to the wood saprobic ascomycete, Auerswaldia lignicola (Family Botryosphaeriaceae), in a carpenter in India. Mycopathologia, 2013. 176(5-6): p. 463-6.
16. Sadeghi Tari, A., et al., Post-traumatic fatal Nattrassia mangiferae orbital infection. International Ophthalmology, 2005. 26(6): p. 247-250.
17. Machouart, M., et al., Scytalidium and scytalidiosis: What’s new in 2012? Journal de Mycologie Médicale, 2013. 23(1): p. 40-46.
