Title: New Blurred Vision and Headaches Occurring Eight Months After Treatment for Cryptococcus neoformans Meningitis in a Non-HIV, Non-Transplant Patient
Submitted by: Lana Abusalem, MD; Julia Messina, MD, Molly Hillenbrand, MD
Institution: Duke University, Division of Infectious Diseases
Email: lana.abusalem@duke.edu
Date Submitted: 5/31/2024
History:
A 28-year-old man from North Carolina presents with headaches, expressive aphasia, and seizures eight months after diagnosis with Cryptococcus neoformans meningitis. Regarding his initial presentation with Cryptococcus meningitis, he presented with dyspnea, difficulty walking, and expressive aphasia. After extensive work up, lung biopsy showed granulomas, brain MRI revealed hydrocephalus, and MRI of spine showed diffuse leptomeningeal enhancement with findings concerning for possible neurosarcoid. Lumbar puncture was notable for an elevated opening pressure (LP-OP) of 17mmHg, neutrophilic pleocytosis (56-58 WBC cells/mm3, 56-64% neutrophils) and elevated protein (263 mg/dL). Cerebrospinal fluid (CSF) Biofire panel was negative, but a separate CSF Cryptococcal antigen (CrAg) was not done.
CSF angiotensin converting enzyme (ACE) levels were elevated, so the patient was started on prednisone 80mg daily and methotrexate 10mg PO weekly for treatment of neurosarcoid. The patient then presented several weeks later with bilateral upper extremity shaking concerning for seizures and underwent a stroke evaluation. Repeat MRI brain showed increased hydrocephalus. LP-OP was once again elevated at 28 mmHg, WBC 12 cells/mm3, glucose <10 mg/dL. CSF CrAg titers came back positive at 1:640, serum CrAg titer was >1:2560 with positive CSF culture for Cryptococcus neoformans. He was treated initially with liposomal amphotericin B 5 mg/kg every 24 hours and flucytosine 25 mg/kg/dose every 6 hours for induction therapy but self-discharged after a week of therapy. He was advised to taper off his prednisone by 10mg every week to a dose of 10mg prednisone once daily.
Over the next two months, the patient had multiple readmissions for worsening headaches and elevated intracranial pressure; he underwent repeat evaluation with LP-OP as high as 30 mmHg during one admission but often self-discharged before completing treatment. Eventually, he underwent ventriculoperitoneal (VP) shunt placement. CSF cultures were negative by this time, and he completed two weeks of induction therapy with liposomal amphotericin B and flucytosine approximately 2 months after the initial positive CSF culture. The patient was subsequently transitioned to fluconazole therapy. It is worth noting that the patient began experiencing cognitive decline and disorientation to timeline of events as early as four months into his diagnosis of Cryptococcus meningitis.
Immunologic work-up was performed for underlying immunodeficiencies contributing to his Cryptococcus meningitis, He was eventually diagnosed with common variable Immune deficiency (CVID) 6 months after his initial presentation and was subsequently tapered off the PO prednisone 10mg once daily over 7 days. His neurosarcoid diagnosis was reevaluated and also suspected to be a true diagnosis, likely contributing to his symptoms and predisposition to meningitis.
The patient now presents with new bilateral blurring of vision with headaches approximately 10-14 days after stopping PO prednisone, prompting an MRI of the brain and orbits with and without contrast. He initially reported difficulty reading subtitles on his hospital room TV with worsening blurred vision. Had denied floaters, blind spots, focal weakness in either of his extremities or hearing disturbances. He denied new chills, fevers, nausea or vomiting. Ventriculoperitoneal shunt was evaluated by neurosurgical teams and was noted to be properly calibrated and functional without obstruction.
Physical Examination:
T: 98.6. BP: 132/70. HR 95. Breathing on room air.
General: alert, cooperative, in not acute distress
HENT: oropharynx clear, moist mucous membranes, good dentition, no oral ulcers or exudates.
Chest/Cardiovascular: regular rate and rhythm, without murmurs, rubs or gallops
Respiratory: clear to auscultation, good air exchange
GI/Abdomen: soft, nontender, nondistended. Purple striae noted on abdomen.
Extremities: no lower extremity edema
Skin: no rashes, clean peripheral IV sites
Neurologic: alert, oriented to self and location, disoriented to time.
Pupils equal, round, and reactive. Able to read large text on the TV in his room, visual acuity on Snellen-Linear chart was 20/30 in right eye, 20/30 in the left (reduced from 20/20 3 weeks prior). Peripheral vision, color vision and visual fields were intact. Fundoscopy notable for normal rim, and no blurring of disc margins bilaterally, Cup to Disc (C/D) ratio was 0.3 bilaterally.
CN III-XII intact. Intact strength in the bilateral upper/lower extremities (power 5/5) and intact sensation to light touch throughout.
Laboratory Examination:
Sodium 135 (Reference Range: 135-145 mmol/L)
Potassium 3.2 (Reference Range: 3.5-5 mmol/L)
Serum Creatinine 0.7 (0.6-1.3 mg/dL, at baseline)
AST 13 (Reference Range: 15-41 U/L)
ALT 18 (Reference Range: 15-50 U/L)
Total Bilirubin 1.1 (Reference Range: 0.4-1.5 mg/dL)
WBC 4.5; ranged between 2.8-4.9. (Reference Range: 3.2-9.8×10^9/L)
Hemoglobin 10.3 (Reference Range: 13.7-17.3 g/dL)
Platelets 219 (Reference Range: 150-450 g/dL)
ESR and CRP within normal limits.
Question 1: What are probable/possible diagnoses?
Given his history, emergence of new symptoms of blurred vision and headaches despite properly functioning VP shunt and having completed induction treatment for Cryptococcus meningitis with documented CSF clearance with transition to fluconazole, the differential diagnosis at this time included relapsed Cryptococcus meningitis, hospital-acquired meningitis, new hospital acquired infection or viral respiratory illness, or neuro-sarcoidosis flare after steroid tapering. His symptoms were not consistent with his initial presentation, and occurred approximately two weeks after steroids were completely tapered off. Moreover, the timeline of his symptoms this far out from a Cryptococcus treatment course, and new blurred vision raised concerns for post-infectious inflammatory response syndrome (PIIRS).
Microbiology/Diagnostic Tests Performed:
Microbiology:
-HIV Antibody-Antigen testing: Negative
-Lumbar Puncture Results:
| at initial presentation | -LP-OP of 17 mmHg -Neutrophilic pleocytosis (56-58 WBC cells/mm3, 56-64% neutrophils) -Elevated protein (263 mg/dL) -CSF Biofire panel was negative, separate CSF cryptococcal Antigen (CrAg) was not done. -CSF ACE levels were elevated at 7.6-8.4 U/L (Reference Range: 0-2.5 U/L). |
| one month later, at initial Cryptococcus Meningitis diagnosis | -LP-OP 28 mmHg -WBC 12 cells/mm3 -Glucose <10 md/dL -Positive CSF CrAg titers at 1:640 -Positive CSF culture for Cryptococcus neoformans |
-Serum Cryptococcal Antigen: positive with titers >1:2560 at diagnosis and remained persistently >1:2560 throughout his course.
Imaging:
-Lumbar Spine MRI with Contrast:
Diffuse thickening and enhancement involving the length of the visualized spinal canal, including the cauda equina nerve roots.
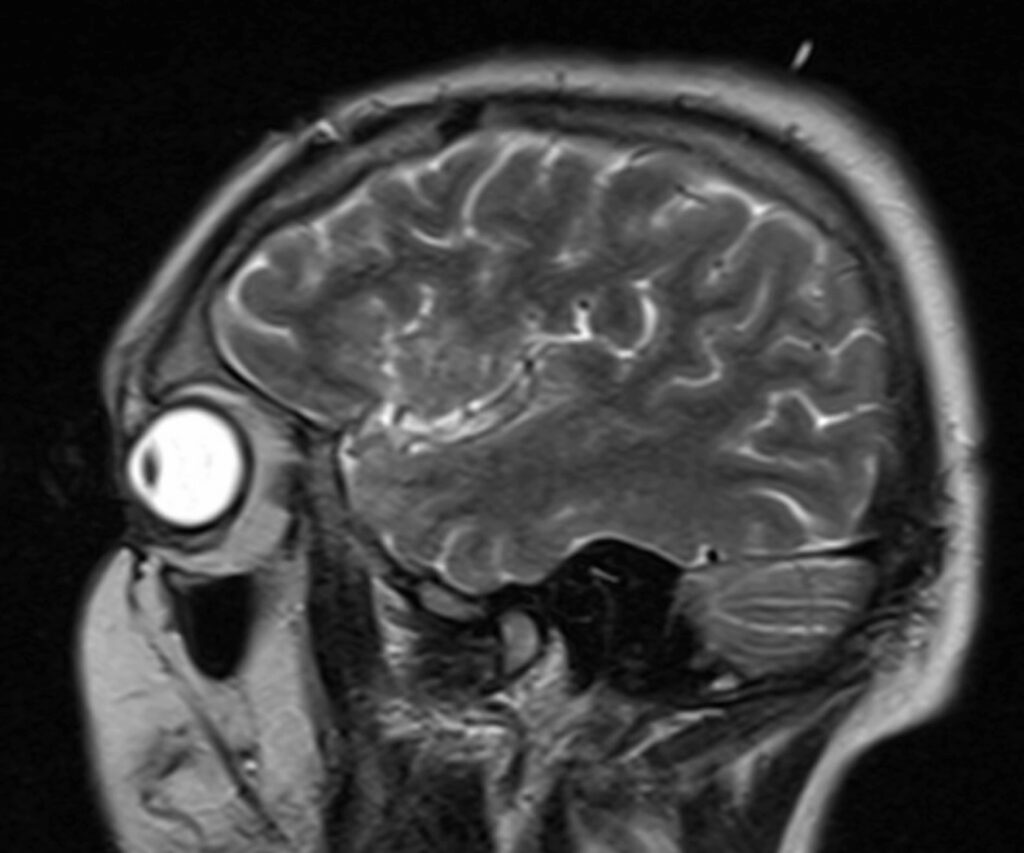
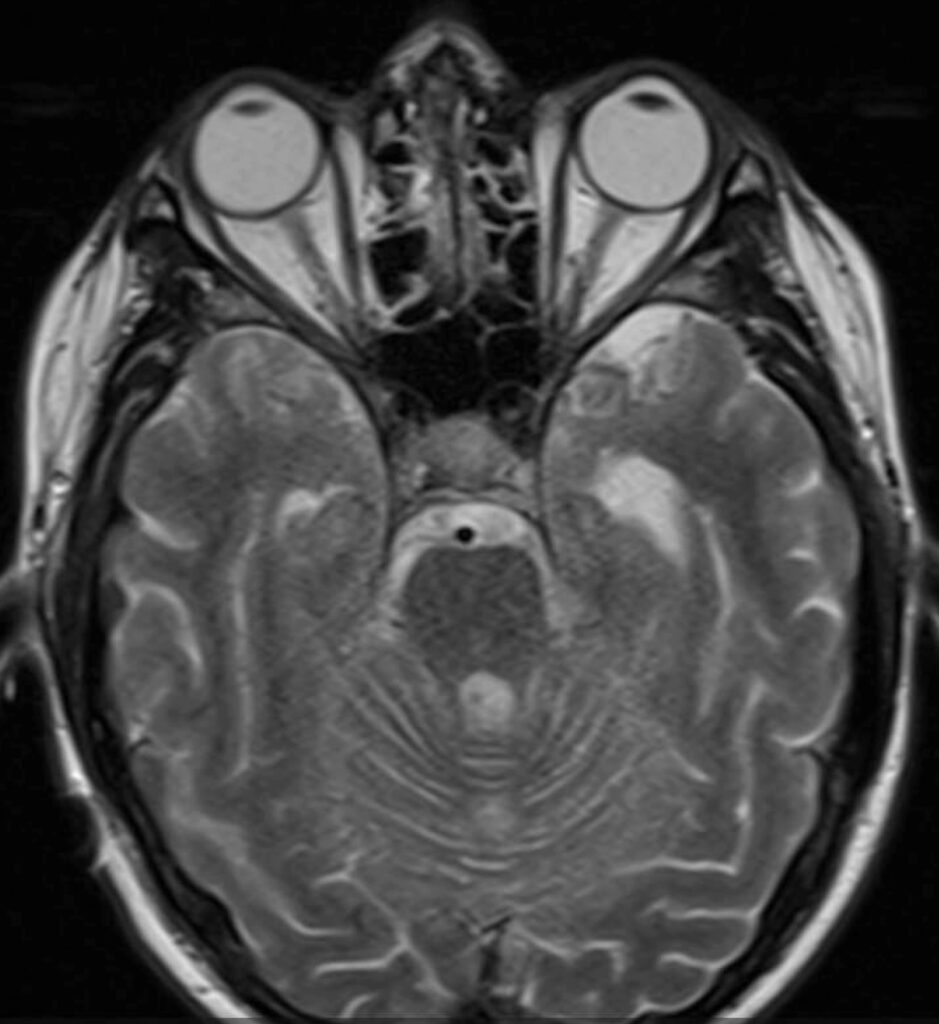
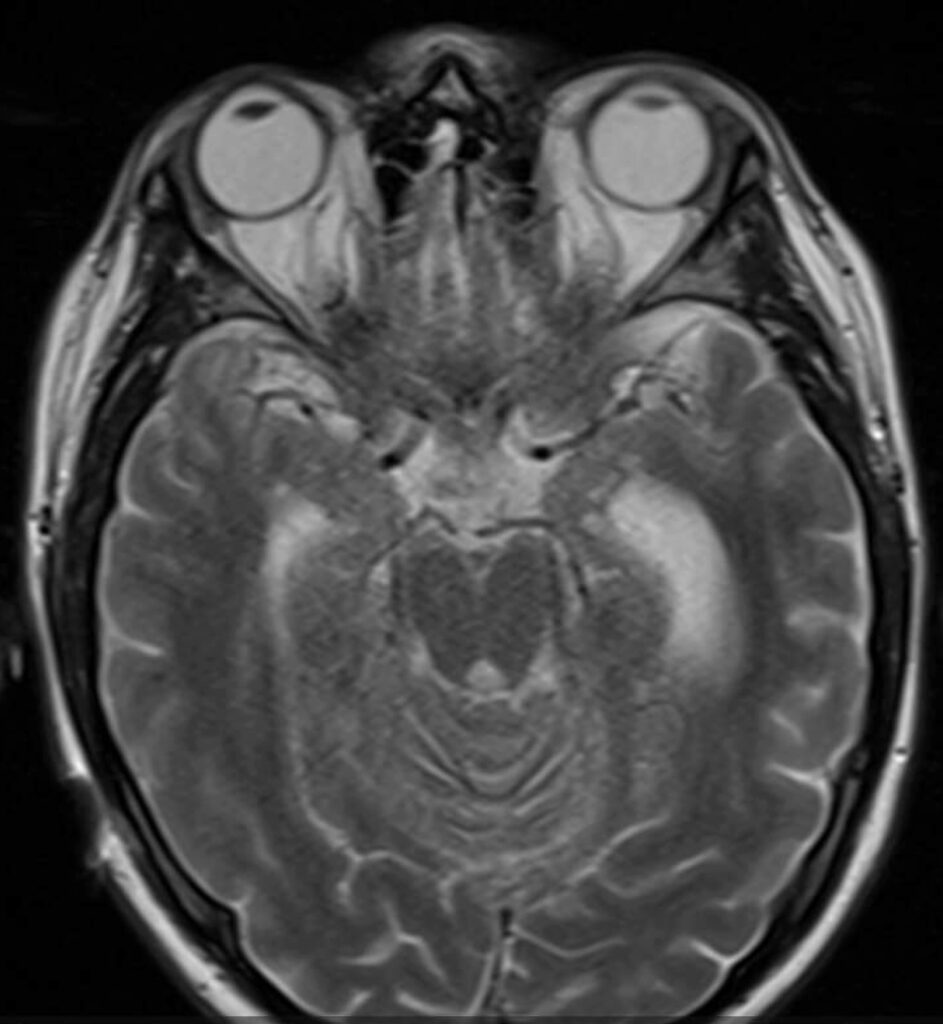
-Orbit and Brain MRI with and without Contrast: [Refer to Images 1-3].
Substantial worsening in diffuse, extensive leptomeningeal contrast enhancement compared to MRI obtained 2 months prior including involvement of the optic chiasm, optic tracts and intracranial portion of the optic nerves.
Immunology Evaluation:
-Lymphocyte enumeration panel with absolute lymphopenia (260) with normal distribution of T, B, and NK cells.
-B-cell phenotyping showed low percentage of class switch memory B cells (5.5% of CD27+ CD19+ B cells).
-Immunoglobulin profile with low IgG 438 (previously normal at 690 approximately 1 year prior), low IgM 32, normal IgA 75, and undetectable IgE.
-Tetanus toxoid antibodies were protective.
-Pneumococcal titers were protective to 7 of the 23 serotypes
-Cellular immunocompetence profile showed normal proliferation response to
Phytohemagglutinin and Concanavalin A mitogens (T-cell dependent Mitogens) but reduced response to Pokeweed mitogen consistent with CVID
-Invitae primary immunodeficiency panel revealed an increased risk heterozygous variant in NOD2 (p.Arg702Trp).
Final Diagnosis: Post Infectious Inflammatory Response Syndrome (PIIRS)
Question 2: What treatment is recommended in the care of this patient?
Treatment: The patient was started on 1 mg/kg/day prednisone and was eventually discharged on 60 mg prednisone once daily for at least one month with plans for very prolonged taper as per his clinical course.
Outcome: Improvement in symptoms, with resolution of ocular symptoms after initiation of steroid therapy. The patient was eventually discharged home on hospital day 51, approximately three weeks after steroid initiation. He also received one dose of Intravenous Immunoglobulin (IVIG) prior to discharge with plans to give IVIG 500mg/kg every 28 days outpatient for his CVID.
Discussion: (500 words)
Cryptococcus neoformans, a neurotropic yeast that primarily infects the lungs and can cause disseminated disease, has been described in HIV-positive patients, transplant recipients, and seemingly immunocompetent patients often categorized as non-HIV, non-Transplant patients[1]. The 2010 Infectious Diseases Society of America (IDSA) cryptococcal Guidelines categorize induction treatment recommendations based on the above distinct groups, in recognition of the shift in susceptible host characteristics over time particularly with the increased use of Anti-Retroviral Therapy (ART), increased stem cell and solid organ transplantations and the variability in disease presentation, course and outcomes[1,2,3]. HIVnegative patients with cryptococcosis are more likely to develop long-term neurological sequalae[4]. Moreover, HIV-negative, non-transplant patients are more likely to have longer duration of symptoms, more severe cryptococcal disease, and increased all-cause mortality. [1,5]. This category of HIV-negative, non-transplant patients includes those with impaired cellmediated immunity, immunoglobulin disorders such as CVID, those on chronic glucocorticoid therapy and some disease modifying agents, and hematological malignancies[1,3]. Seemingly immunocompetent patients otherwise may still have underlying macrophage dysfunction increasing their risk of invasive Cryptococcus disease [6]. There is often a delay in diagnosis in this subset of patients and subsequently an increased risk of therapeutic failure and worse prognosis, so a high index of clinical suspicion needs to be utilized and evaluation for underlying immunodeficiencies should be considered [2,5]. They are also more likely to have a dysregulated vigorous inflammatory response than patients with HIV or history of transplantation [5,6]. Although immune reconstitution inflammatory syndrome (IRIS) has been well documented in patients with HIV and cryptococcosis and sterile CSF cultures, it is often associated with institution of ART and subsequent rapid improvement in immune function. A similar phenomenon has been observed in non-HIV patients but due to other forms of immune dysregulation and in response to the release of fungal antigens during therapy [7]. Often misdiagnosed as recurrence of cryptococcosis or failed antifungal treatment due to persistently elevated serum cryptococcus antigens, patients characteristically have sterile CSF cultures and develop symptoms within 20-40 days from initiation of induction therapy. [8]. Williamson et al have coined this syndrome of deteriorating mental status and function or “refractory disease” after 1 month of Amphotericin-based therapy and despite negative CSF cultures, as post-infectious inflammatory response syndrome (PIIRS), which is associated with increased T-cell activation, robust IFN-γ response and axonal damage. These patients appear to suddenly worsen, develop severe headaches, increased intracranial pressures and impaired neurological function with the most common symptoms being altered mental status and vision changes; similar to the patient presented in this case [9]. In a case series of 15 previously healthy patients with cryptococcal meningitis and PIIRS, Anjum et al have shown that treating those patients with high-dose intravenous methylprednisolone 1 gm daily for 1 week followed by oral prednisone 1 mg/kg/day (with subsequent taper based on response) in addition to PO fluconazole resulted in improvement in cognitive function, ophthalmic and audiologic exams and MRI findings. This case not only highlights the challenges and diagnostic delays associated with the diagnosis of cryptococcus meningitis in non-HIV, non-transplant patients but also the increased risk of adverse outcomes and complications including PIIRS in this subset of Cryptococcus meningitis patients.
Key References:
1. Bratton EW, El Husseini N, Chastain CA, et al. Comparison and temporal trends of three groups with cryptococcosis: HIV-infected, solid organ transplant, and HIVnegative/non-transplant. PLoS One. PMID: 22937064
2. Perfect JR, Dismukes WE, Dromer F, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin Infect Dis. PMID: 20047480
3. Aberg JA, Mundy LM, Powderly WG. Pulmonary cryptococcosis in patients without HIV infection. Chest. PMID: 10084485.
4. Marr KA, Sun Y, Spec A, Lu N, et al; Cryptococcus Infection Network Cohort Study Working Group. A Multicenter, Longitudinal Cohort Study of Cryptococcosis in Human Immunodeficiency Virus-negative People in the United States. Clin Infect Dis. PMID: 30855688
5. Brizendine KD, Baddley JW, Pappas PG. Predictors of mortality and differences in clinical features among patients with Cryptococcosis according to immune status.PMID: 23555970.
6. Williamson PR. Post-infectious inflammatory response syndrome (PIIRS): Dissociation of T-cell-macrophage signaling in previously healthy individuals with cryptococcal fungal meningoencephalitis. Macrophage (Houst). PMID: 27064474.
7. Decote-Ricardo D, LaRocque-de-Freitas IF, Rocha JDB, Nascimento DO, Nunes MP, Morrot A, Freire-de-Lima L, Previato JO, Mendonça-Previato L, Freire-de-Lima CG. Immunomodulatory Role of Capsular Polysaccharides Constituents of Cryptococcus neoformans. Front Med (Lausanne). PMID: 31275938.
8. Wu G, Guo X, Wang Y, Hu Z. Clinical and Radiographic Features of Cryptococcal Neoformans Meningitis-associated Immune Reconstitution Inflammatory Syndrome. PMID: 32561831.
9. Anjum S, Dean O, Kosa P, et al. Outcomes in Previously Healthy Cryptococcal Meningoencephalitis Patients Treated With Pulse Taper Corticosteroids for Postinfectious Inflammatory Syndrome. Clin Infect Dis. PMID: 33383587
Images and Figures:
1- Images 1-3: Brain and Orbit MRI with leptomeningeal enhancement of the optic chiasm, optic tracts and intracranial portion of the optic nerves.
