Title: 88yo Female with fungal sinus infection and skull osteomyelitis
Submitted by: Julia Schroeder, Christine Hsu, Lindsey Hastings, Emily Wong, Sixto Leal, Peter G. Pappas
Institution: UAB
Email: ppappas@uabmc.edu
Date Submitted: 6/24/24
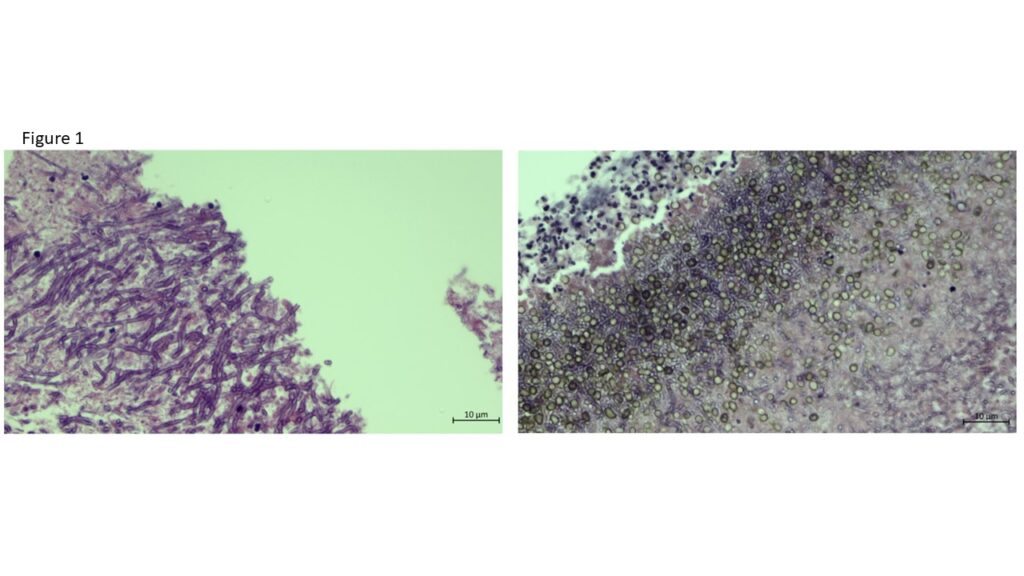
An 88-year-old female with hemochromatosis and cirrhosis presented with persistent left-sided otalgia, decreased hearing, and occipital headaches for several months. Despite ear tube placement, symptoms persisted, with additional sinus congestion and neck pain. She did not have any fevers, chills, diplopia, or facial numbness. CT sinus showed soft tissue thickening/mass in the left nasopharynx, extending to the occipital condyle and encasing the left internal carotid artery. Nasal endoscopy and initial biopsy was inconclusive. However, repeat biopsy revealed fibrosis, necro-inflammatory debris, mycetoma, and evidence of invasive and non-invasive fungal elements. GMS stain revealed a hyaline-septate mold with pigmented spores.
PMH:
- HTN, HLD, chronic back pain, hypothyroidism, hemochromatosis, cirrhosis
- Meds: HCTZ, diltiazem, lisinopril, levothyroxine, atorvastatin, saline nasal spray
- Surgical Hx: bilateral TKA (2004), L ear tube, nasal endoscopy w/ biopsy (3/21/24), skull base tumor biopsy (4/22/24)
- Family Hx: HTN
- Social Hx:
- Lives in central Alabama
- Tobacco: former smoker (quit in 1996)
- EtOH: denies
- Illicit drugs: denies
HPI:
- 88 yoF w/ hx of HTN, hemochromatosis, and cirrhosis who p/w >5 months of L ear pain, decreased hearing, and occipital headaches
- Developed L ear pain in December of 2023 and had a L ear tube placed
- In January 2024 she developed sinus congestion, neck pain, and decrease visual acuity (attributed to macular degeneration)
- CT on 3/12/2024 showed infiltrating soft tissue thickening/mass at the left nasopharynx encasing the left internal carotid artery
- On 3/23/24 she underwent nasal endoscopy and biopsy – unable to obtain enough tissue
- CT Sinus 4/19: Edematous changes and soft tissue swelling in the nasopharynx, extending into the skull base structures c/f osteomyelitis
- On 4/22 she underwent another biopsy of “skull base tumor” and intra-op tissue was necrotic
- Denies fevers, chills, night sweats, diplopia, facial numbness/weakness
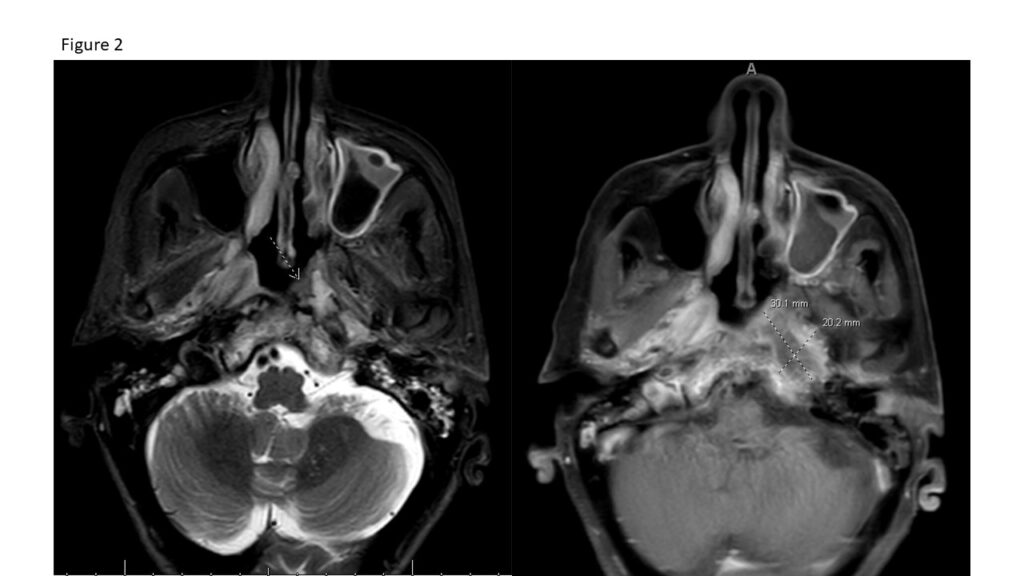
Patient was admitted for invasive fungal sinusitis and was started on lipid formulation of amphotericin B (LFAmB). Clinical examination noted bilateral hearing impairment. Initial admitting labs are depicted below. MRI revealed a heterogeneously enhancing mass lesion involving the left nasopharynx measuring 3 x 2.2 cm, features concerning for skull base osteomyelitis, and diffuse opacification of the left maxillary, ethmoid, sphenoid, and frontal sinuses. On hospital day 7 she underwent resection of the left skull base infection and anterior cranial fossa. Intraoperatively, there was necrotic tissue encountered and debridement was extended all the way to the left internal carotid artery. Pathology from this debridement revealed fungal elements and necrotic debris, but no clear tissue invasion. On hospital day 8, LFAmB was transitioned to isavuconazole given clinical stability. Isavuconazole was chosen over voriconazole to minimize hepatotoxicity in the setting of cirrhosis.
Physical Examination:
- Vitals
- Temp 97.8, HR 66, RR 18, O2 96% on RA, BP 132/61
- Exam
- Gen: NAD, well-appearing
- HEENT: PERRL, EOMI, anicteric sclerae, hearing decreased bilaterally, no sinus tenderness
- CV: RRR, no murmur, no edema
- Resp: CTAB, breathing comfortably on RA
- GI: soft, non-distended, non-tender
- Skin: no rash
- Neuro: alert, oriented, decreased hearing, no other cranial nerve deficits
Laboratory Examination:
Na 134
K 4.4
CL 100
Co2 27
BUN 26
*Creat. 1.3
WBC 5.48
*Hgb 10.8
*HCT 32
*PLT 122
Alk Phos 97
ALT 11
AST 17
T. Bili 0.6
D. Bili 0.1
Albumin 3.7
A1c 5.5
HIV- Neg
*FE 25
*TIBC 267
*% Sat 9
Ferritin 18
Question 1: What are probable/possible diagnoses?
Microbiology/Diagnostic Tests Performed:
- Skull base biopsy: Granulation tissue, fibrosis, necro-inflammatory debris, and mycetoma
- Lateral sphenoid biopsy: Sino-nasal mucosa with chronic inflammation and fibrosis
- Sinus contents excision: Chronic inflammation and fibrosis
- Addendum: GMS highlights invasive and non-invasive fungal elements. The morphology is consistent with hyaline septate hyphae. (Fig 1)
- All cultures for fungi were negative.
MRI Scan (Fig 2)
- Heterogeneously enhancing mass lesion involving the left nasopharynx measuring 3 x 2.2 cm
- Features are concerning for skull base osteomyelitis
- Diffuse opacification of the left maxillary, ethmoid and frontal sinuses, likely from the postsurgical changes
- Diffuse opacification of the left sphenoid sinus, likely proteinaceous collection
CT Scan (Fig 3)
- Hyperdense secretions throughout the left frontal drainage pathways, sphenoid sinuses, and ethmoid sinuses
- Opacification and erosive changes involving the left mastoid cells and opacification of the left middle ear, possible otomastoiditis

Hospital Course
- On 5/6 underwent resection of skull base infection, anterior cranial fossa, left resection of skull base infection, and anterior cranial fossa
- Was continued on amphotericin from 5/1-5/8 -> switched to isavuconazole
Pathology
- Left skull base, debridement: Fungal elements within necrotic debris
- Left lateral sphenoid, debridement: Chronic inflammation
- Left vidian nerve, debridement: Chronic inflammation
- Sinus contents, debridement: Sinonasal mucosa with acute and chronic inflammation, necro-inflammatory debris and mucin, scant bone fragments appear viable
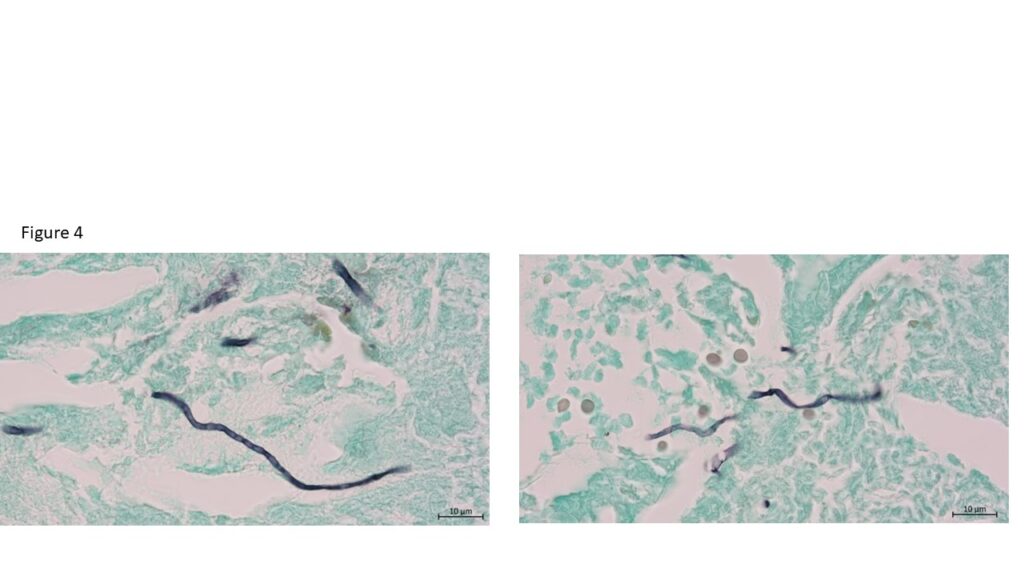
- Addendum: GMS highlights fungal elements in blood clot, mucin, and acellular debris
- (Figure 4) NGS (16s) Scedosporium boydii (also known as Pseudallescheria boydii) or Scedosporium apiosperum
- (Figure 5)
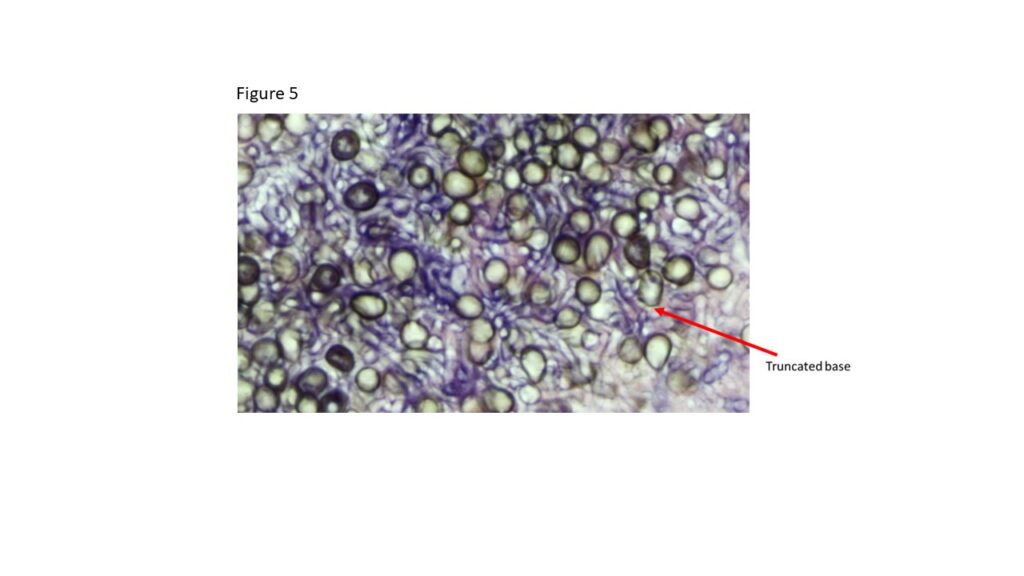
Final Diagnosis: Scedosporium boydii
Question 2: What treatment is recommended in the care of this patient?
Treatment: LFAmB from 5/1-5/8 -> switched to isavuconazole
Outcome: The patient reported a progressive improvement in pain. She was discharged after two weeks on isavuconazole 372 mg daily. Follow up was arranged for 2 months following discharge.
The fungal cultures taken from the sinus and skull base tissue remained negative throughout her course, and NGS sequencing was submitted to identify the causative organism.
Discussion:
- Acute IFS:
- Poorly controlled diabetes or profound immunosuppression
- Time course: days to a few weeks
- Hyphal invasion of blood vessels with resulting tissue infarction
- Aspergillus species, Fusarium species, and the Mucorales
- Chronic IFS:
- Immunocompetent or less immunocompromised
- Time course: >12 weeks
- fungal invasion of the submucosa associated with chronic inflammation and fibrosis
- Dematiaceous molds (Bipolaris, Curvularia, and Alternaria spp), Aspergillus spp, Scedosporium apiospermum complex
Treatment:
- Empiric antifungal therapy (typically amphotericin B)
- Urgent surgical evaluation for biopsy and debridement
- Radical surgical debridement is typically required to achieve cure
- Restoration of immune function by withdrawal of immunosuppressive medications, control of metabolic perturbations, and control of the underlying illness
- Intravenous therapy is typically continued until there is clear clinical response
- Suppressive therapy is usually continued for at least 3-6 months
- Some patients who remain immunocompromised require lifelong therapy
Scedosporium apiospermum complex
- Causes sinusitis, pneumonia, and disseminated infections in immunocompromised hosts and mycetoma in immunocompetent patients
- Associated with near-drowning
- Deeply invasive infections carry a high mortality
- Pneumonia due to S. apiospermum is clinically indistinguishable from that due to Aspergillus
- Voriconazole is treatment of choice
- Amphotericin is not effective
Isavuconazole versus voriconazole for primary treatment of invasive mold disease caused by Aspergillus and other filamentous fungi (SECURE): a phase 3, randomized-controlled, non-inferiority trial
- Compared the efficacy and safety of voriconazole and isavuconazole for the treatment of invasive aspergillosis and other mold infections
- Study demonstrated that isavuconazole is non-inferior to voriconazole in patients suspected of having invasive mold disease
- Isavuconazole group had significantly fewer drug-related adverse events and fewer drug discontinuations
Key References:
- Thompson GR, 3rd, Patterson TF. Fungal disease of the nose and paranasal sinuses. J Allergy Clin Immunol. Feb 2012;129(2):321-6. doi:10.1016/j.jaci.2011.11.039
- Aribandi M, McCoy VA, Bazan C, 3rd. Imaging features of invasive and noninvasive fungal sinusitis: a review. Radiographics. Sep-Oct 2007;27(5):1283-96. doi:10.1148/rg.275065189
- Khoueir N, Verillaud B, Herman P. Scedosporium apiospermum invasive sinusitis presenting as extradural abscess. Eur Ann Otorhinolaryngol Head Neck Dis. Apr 2019;136(2):119-121. doi:10.1016/j.anorl.2018.11.009
- Maertens JA, Raad, II, Marr KA, et al. Isavuconazole versus voriconazole for primary treatment of invasive mould disease caused by Aspergillus and other filamentous fungi (SECURE): a phase 3, randomised-controlled, non-inferiority trial. Lancet. Feb 20 2016;387(10020):760-9. doi:10.1016/S0140-6736(15)01159-9
- Connor RF. Treatment of Scedosporium and Lomentospora infections. UpToDate.
