History:
62 y/o man with cirrhosis, presented to the emergency department with the chief complaint of fatigue, dizziness, weight loss, and a tongue lesion. Over the preceding 6 months he states he has had progression of his current symptoms and sought care only after the development of a tongue lesion he noticed 3 weeks prior. He states this lesion is moderately painful particularly while eating or drinking. He has not noticed any discharge from this lesion and it has slowly enlarged. During this time frame he has lost over 80 lbs and he additionally complains of mild shortness of breath and a scant, dry cough. He denies fever, chills or sweats. He has no headache or vision changes. He denies chest pain or palpitations, and has no abdominal pain, diarrhea, constipation, joint pain, or skin rashes.
Physical Examination:
Temp: 37.5.1 °C | BP: 105/65 mmHg Pulse: 80 | Resp: 17 | SpO2: 85 % Weight: 60 kg
- General Appearance: alert, in no distress
- Eyes: conjunctivae and corneas clear. PERRL, EOM’s intact.
- Mouth: oropharynx clear. Two discrete lesions on tongue, one nodular the other ulcerative (fig 1). These were moderately painful to palpation
- Heart: S1/S2 regular, no murmurs.
- Lungs: clear to auscultation bilaterally.
- Abdomen: soft and non-tender, normal bowel sounds x 4
- Extremities: no edema
- Skin: no rashes, lesions.
- Mental Status: alert and fully oriented.
- Musculoskeletal: no joint swelling.

Figure 1
Laboratory Examination:
- CBC: WBC 12.0 with normal differential, platelets of 205
- CMP: Na 123, K 5.0, Cl 92, CO2 29, BUN 15, Cr 1.1, Gluc 102
- LFTs: AST 75, ALT 65, ALP 554, ALB 3.0, TBIL 1.3
Question:
What further diagnostic testing and treatment are recommended for this patient?
Answer and Discussion
Biopsy of the tongue and assessment of adrenal insufficiency.
Biopsy of the tongue and culture showed Histoplasma spp. (Figure 2).
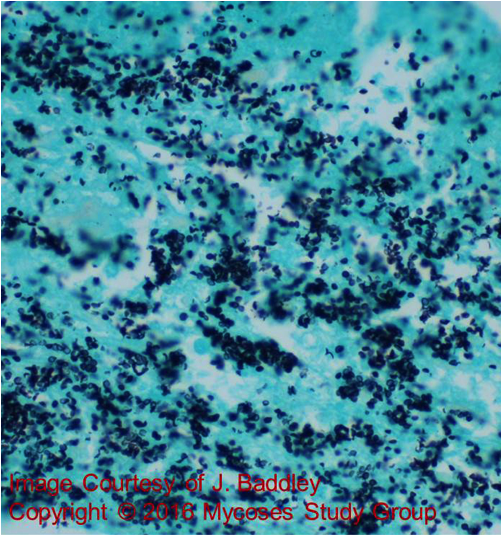
Figure 2
Adrenal insufficiency was confirmed and imaging of the abdomen revealed enlarged adrenal glands bilaterally from infection with Histoplasma (Figure 3).
Urinary Histoplasma antigen testing was positive: 2.97 ng/ml
Histoplasmosis within North America is caused by the endemic mycosis, Histoplasma capsulatum. Within the United States infection is most common throughout the Midwest, and within the Ohio and Mississippi River Valley although infection is also seen in non-traditional areas (1).
Disseminated infection occurs through hematogenous spread and the majority of patients who develop this complication have underlying immunosuppression (AIDS, solid organ transplant, or are receiving anti-TNF? therapy). Patients with widespread dissemination typically present with fever, fatigue, hepatosplenomegaly, and pancytopenia. Gastrointestinal disease occurs in ~70% of patients with dissemination (2), while adrenal involvement is equally common (80-90% of autopsied cases) (3).

Figure 3
Diagnostic testing depends on the timing and the extent of infection. In those with disseminated infection, such as the case presented, urinary Histoplasma antigen testing is almost always positive and is useful to follow during therapy. In those with acute or localized pulmonary disease, the sensitivity of urinary antigen decreases and combined serum antibody and urine antigen testing is often needed.
Treatment for patients with dissemination typically consists of an amphotericin B formulation pending clinical improvement. Following a response to therapy, oral itraconazole is recommended (4). The response rate for primary therapy with itraconazole in early studies was 100% for disseminated histoplasmosis and 80% for pulmonary histoplasmosis (5). The oral capsule formulation or the solution can be used. Therapeutic drug monitoring (TDM) of itraconazole is recommended to ensure adherence, and adequate serum drug levels are achieved. Fluconazole appears to be less effective than itraconazole during treatment, and although posaconazole, voriconazole, and isavuconazole have demonstrated in vitro activity against Histoplasma spp, clinical evidence is limited.
Key References:
- Benedict K, Thompson GR, 3rd, Deresinski S, Chiller T. Mycotic Infections Acquired outside Areas of Known Endemicity, United States. Emerg Infect Dis. 2015 Nov;21(11):1935-41.
- Assi MA, Sandid MS, Baddour LM, Roberts GD, Walker RC. Systemic histoplasmosis: a 15-year retrospective institutional review of 111 patients. Medicine (Baltimore). 2007 May;86(3):162-9.
- Goodwin RA, Jr., Shapiro JL, Thurman GH, Thurman SS, Des Prez RM. Disseminated histoplasmosis: clinical and pathologic correlations. Medicine (Baltimore). 1980 Jan;59(1):1-33.
- Wheat LJ, Freifeld AG, Kleiman MB, Baddley JW, McKinsey DS, Loyd JE, et al. Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007 Oct 1;45(7):807-25.
- Dismukes WE, Bradsher RW, Jr., Cloud GC, Kauffman CA, Chapman SW, George RB, et al. Itraconazole therapy for blastomycosis and histoplasmosis. NIAID Mycoses Study Group. Am J Med. 1992 Nov;93(5):489-97.
