Title: 60 yo man with cough and severe cachexia
Submitted by: Peter Pappas, MD
Institution: UAB
Email: ppappas@uabmc.edu
Date Submitted: Dec 2020
History of Present Illness:
- 60 yo white male has experienced largely non-productive cough for over 2 years. He reports occasional sputum production and streaky hemoptysis. Has severe DOE with 20 yds walking before becoming SOB.
- Denies fever, but has experienced substantial weight loss of 55 pounds (BL 160#, currently 105#) during this time. Has frequent night sweats. Appetite is poor, no diarrhea or abdominal pain or bloating.
- Denies sick contacts, no known TB exposure, no prison time or illicit drug use
- Uninsured and ‘can’t afford to go to doctors’ but very concerned
Social History:
- Has lived in rural Central Alabama most of his life.
- Works as self-employed trucker, drives locally and statewide.
- Has not worked in mining, sawmills, factories or
- Smokes 2 ppd for 40 years, stopped 3 yrs ago
- Occasional MJ, no other illicit drugs
- Lives alone, 2 dogs and 3 cats, no livestock, no hunting/fishing
Medical History:
- Several recent hospitalizations at a local hospital for pneumonia. Never stayed more than 5 days, has had at least 1 non-diagnostic bronchoscopy for necrotizing pneumonia in February 2019
- H/O COPD on inhaled bronchodilators
- H/O HBP on no meds
- No other recent hospitalizations
- All previous work ups were ‘negative’ according to the patient and review of sparse records (neg routine, AFB, fungal smear and culture, negative cytology)
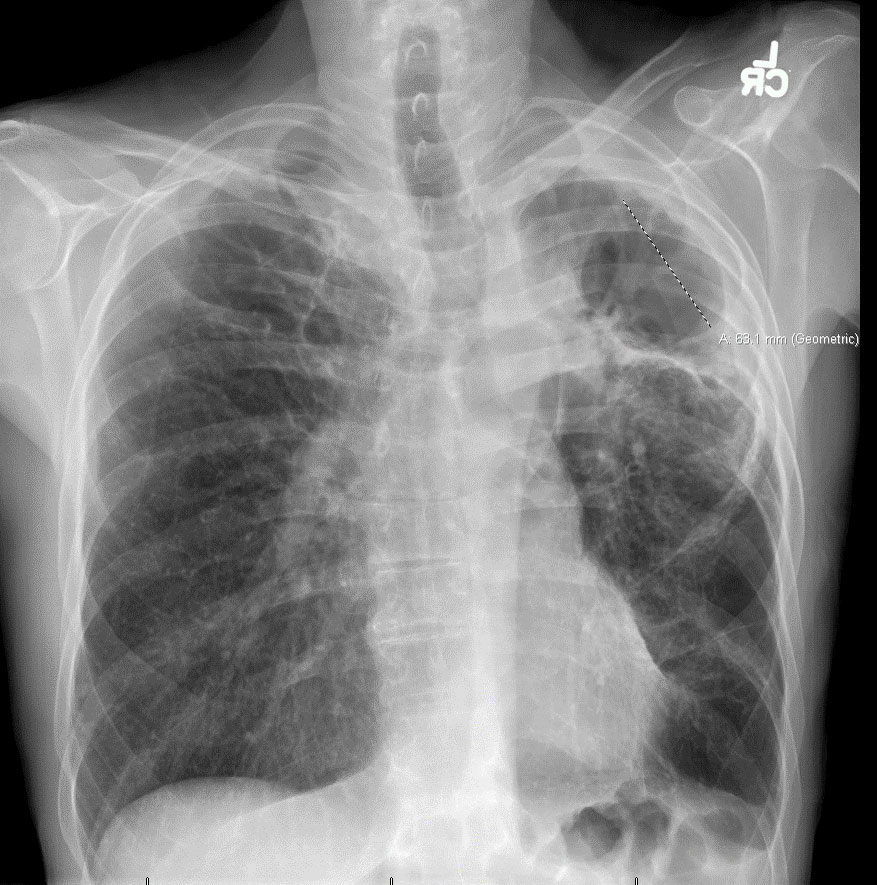
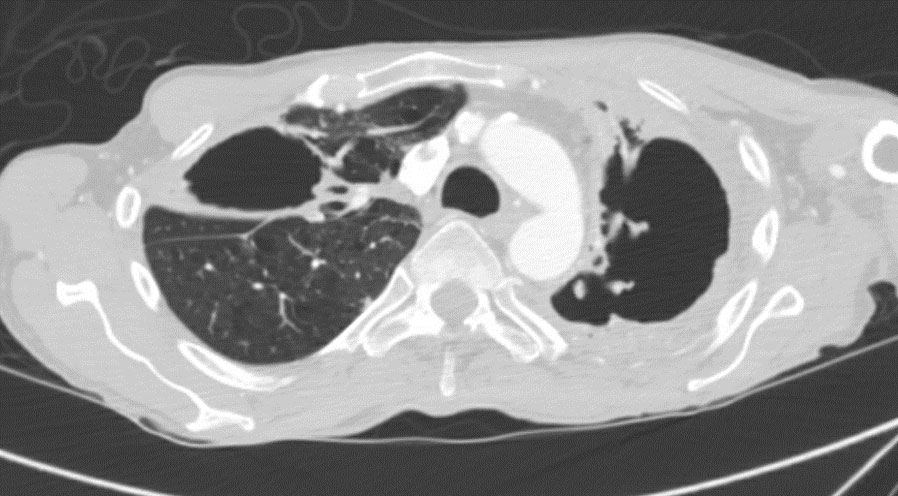
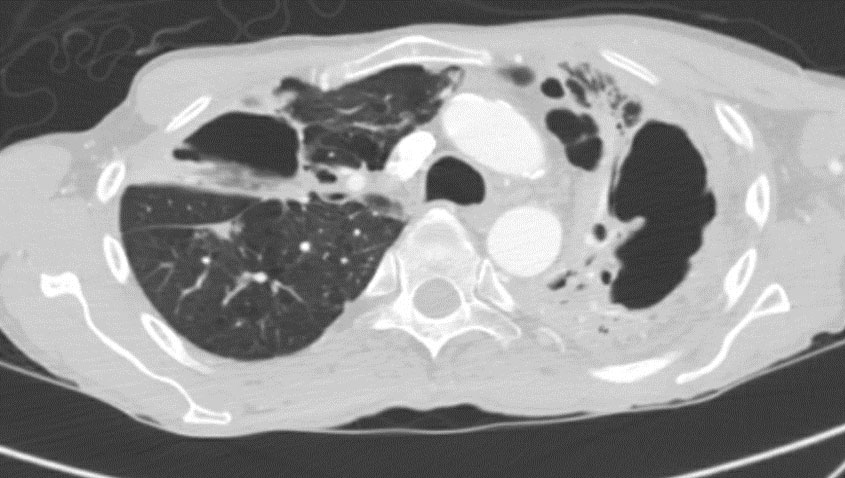
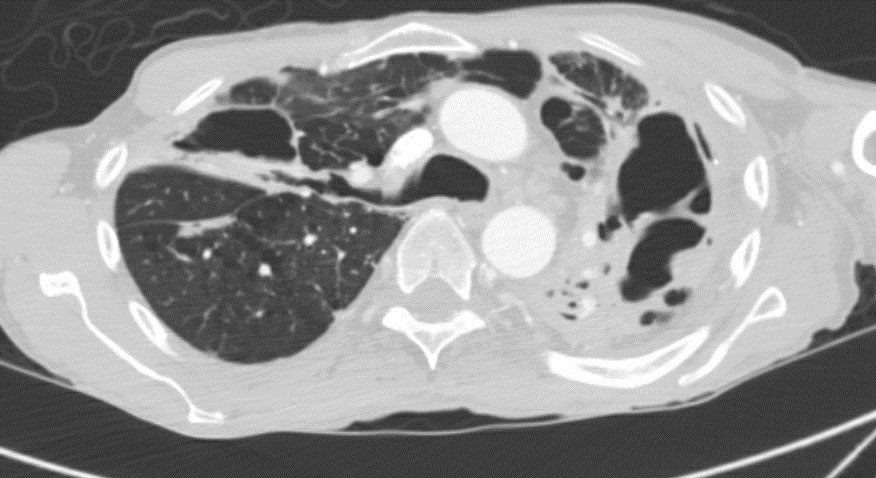
Radiology- See Figures 1-4 These images reveal parenchymal changes consistent with severe COPD, along with biapical thick walled cavitary lesions, much worse on left compared the right apex.
Physical Examination:
- Extremely cachectic elderly white man (wt 105#, Ht 73 inches, BMI 13.85)
- BP 139/90, HR 110, RR 20, T 98°F, O2 Sat 93% RA
- HEENT, Skin, Ext, Abdomen WNL
- Chest with distal breath sounds
- CV ST without murmurs, gallops
- Abd soft no masses
Outpatient Workup:
- He is referred to UAB pulmonary clinic
- After review of records he undergoes bronchoscopy with BAL on February 17, 2020
- Initial studies are negative for AFB, fungi, neoplasia
- Routine cultures are negative
Laboratory Examination:
- HCT 51% WBC 5.3, nl diff, Plt 530K
- LFTs, FBP WNL
- PPD negative
- Histo urine antigen negative
- Crypto antigen negative
Question 1: What are probable/possible diagnoses?
- Non-small cell carcinoma of lung?
- Cavitary tuberculosis?
- Pulmonary MAC?
- Chronic cavitary histoplasmosis?
- Pulmonary nocardiosis?
Microbiology/Diagnostic Tests Performed:
2/17/20 BAL
Gram Positive Cocci 2+
Gram Variable Rods 1+
Gram Negative Cocci 1+
White blood cells 3+
No AFB seen on concentrated smear
2/24/20 results- sputum from BAL
GMS stain for fungi (including Pneumocystis) is negative
3/5/20 results update
Mold, ID to follow
3/14/20 results update
Histoplasma capsulatum
Final Diagnosis: Pulmonary Histoplasma capsulatum
Question 2: What treatment is recommended in the care of this patient?
See: Wheat LJ, Friefeld AG, Kleiman MB, Baddley JW, McKinsey DS, Loyd JE, Kauffman CA. Clinical practice guidelines for the management of patients with Histoplasmosis: 2007 Update by the Infectious Diseases Society of America. CID 2007;45:807-25 (Table 3) https://doi.org/10.1086/521259 (hyperlink to free text journal article)
- Fluconazole?
- Itraconazole?
- Posaconazole?
- Voriconazole?
- Amphotericin B?
- Lipid Ampotericin B?
Treatment: Conventional itraconazole 200 mg po bid, continuously
Outcome: Partial improvement clinically characterized by 30 pound weight gain, diminished cough and stable radiograph.
Discussion: (500 words)
This patient was diagnosed with chronic cavitary histoplasmosis based on positive cultures from bronchoalveolar lavage. Histoplasmosis is a fungal infection that can manifest as pulmonary or disseminated infection after primary infection through the inhalation of spores (Histoplasma capsulatum) from the environment. Spores are found in soil that has been contaminated with bird or bat droppings and the disease prevalence is seen most commonly in the Mississippi and Ohio River Valleys but occurs in other areas worldwide.1-4
