Title: Aspergillus Endocarditis
Submitted by: Philipp Koehler1, Matti Adam2 and Oliver A. Cornely1
Institution: 1University of Cologne, Faculty of Medicine, Department I of Internal Medicine, European Excellence Center for Medical Mycology (ECMM), Cologne, Germany and 2University of Cologne, Faculty of Medicine, Department of Cardiology, Heart Center, Cologne, Germany
Email: philipp.koehler@uk-koeln.de
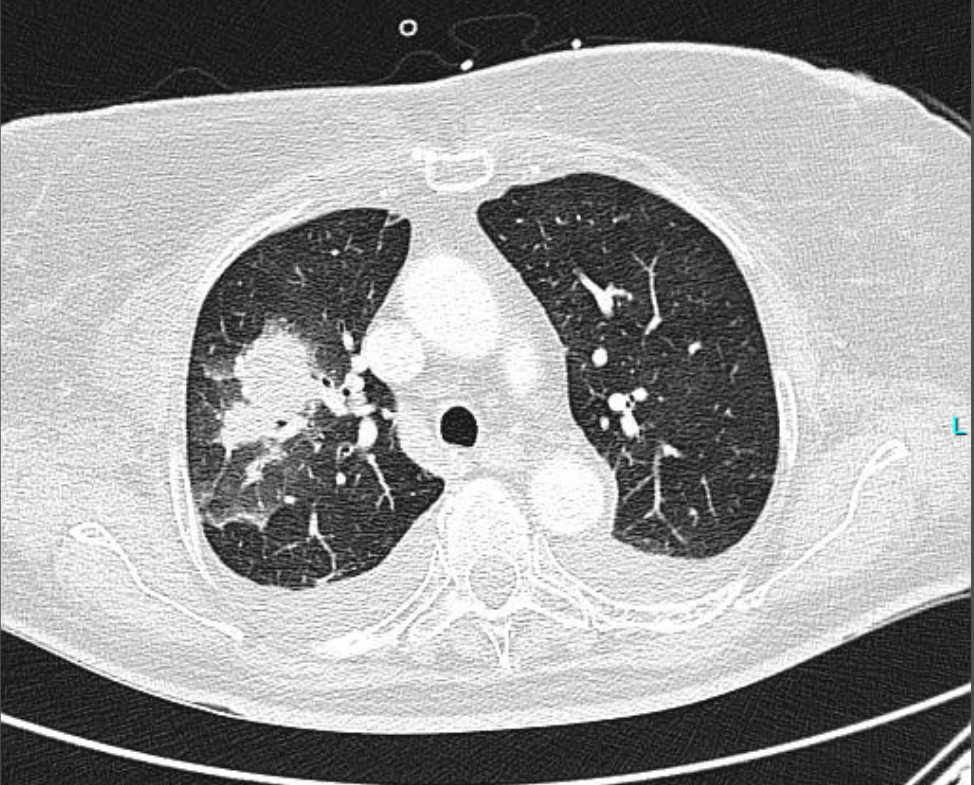
History: A 75 y/o woman was admitted directly to the intensive care unit due to vomiting and diarrhea. Due to repetitive hypertensive crisis, ectopic Cushing syndrome was suspected. The patient also had a steroid induced myopathy and diabetes. During her ICU stay she developed fevers and MRI was suspicious for intrapulmonary lesions that were described as chance findings and prompted a chest CT (Figure 1).
Prior Medical History:Arterial hypertension Mitral valve insufficiency I°Gastric ulcerLiver damage due to alcohol use disorder (withdrawal 20 years before)
Physical Examination:Vital signs: 37.8C, Heart rate 95/min, Respiratory rate: 20/min, Saturation 95% on 4L/min oxygen via maskGeneral state of health: ill appearingHead, Ears, Nose and Throat: anicteric sclera, no palatal lesions
Respiration: left sided rhonchi and weakened breathing sounds
Cardiovascular: regular rate and rhythm, sounds over mitral valve
Skin: well-perfused, warm, dry, no rashes
Laboratory Examination:
| Variable | Reference Range, Adults | Day 5 |
|---|---|---|
| Blood count | ||
| WBCs (x 1E9/liter) | 4.4 – 11.3 | 4.18 |
| RBCs (x 1E12/liter) | 4.0 – 5.2 | 2.7 |
| Hb (g/dl) | 12 – 16 | 8.0 |
| HCT (%) | 36-45 | 23 |
| Platelets (x 1E9/liter) | 150 – 400 | 83 |
| Clinical chemistry | ||
| Sodium (mmol/liter) | 135 –145 | 145 |
| Potassium (mmol/liter) | 3.6 – 4.8 | 2.6 |
| Chloride (mmol/liter) | 94 – 110 | 105 |
| Glucose (mg/dl) | 74 – 109 | 213 |
| Creatinine (mg/dl) | 0.5 – 0.9 | 0.44 |
| Urea (mg/dl) | <50 | 35 |
| Uric acid (mg/dl) | 2.4 – 5.7 | 3.4 |
| AST (sGOT) (U/liter) | <35 | 23 |
| ALT (sGPT) (U/liter) | <35 | 40 |
| GGT (U/liter) | <40 | 112 |
| AP (U/liter) | 35 – 105 | 95 |
| Bilirubin (mg/dl) | <1.2 | 0.3 |
| CRP (mg/liter) | <5.0 | 41.8 |
| PCT (µg/liter) | <0.1 | 0.2 |
| eGFR (CKD-EPI 2009) (ml/min) | 99 | |
Question 1: What are probable/possible diagnoses?
Microbiology/Diagnostic Tests performed: GM serum: 0.1, repetitive Culture of pleural effusion: Klebsiella pneumonia BAL: Klebsiella pneumoniae (Meropenem, gentamicin, ciprofloxacin S), Staphylococcus aureus (MRSA) (Vancomycin, linezolid, daptomycin S) CT guided biopsy: S. aureus PCR negative, Mycobacterium tuberculosis complex PCR negative,
Aspergillus spp. PCR positive, cultures remained negative. Histology (pulmonary lesion): necrotizing pneumonia with proof of fungal hyphae
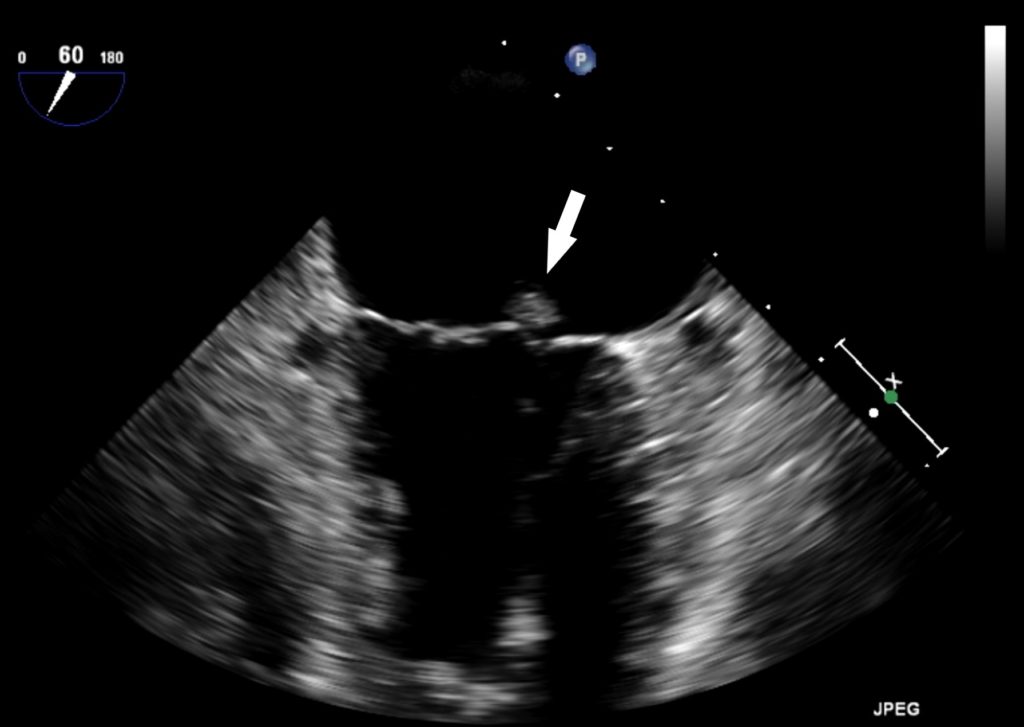
Clinical course: Patient was treated with broad-spectrum antibiotic and antifungal therapy, but fever persisted. Transesophageal echocardiogram was performed, and revealed erosions on the mitral valve (Figure 2), triggering surgical resection of the valve with microbiological work-up. Culture findings: mitral valve – Aspergillus fumigatus, voriconazole (MIC 0.125), amphotericin B (MIC 0.38 mg/L), caspofungin (MIC 0.125) (EUCAST).
Final Diagnosis: Aspergillus endocarditis of the mitral valve, invasive pulmonary aspergillosis and abscess-forming pneumonia by Klebsiella pneumonia and Staphylococcus aureus (MRSA) Treatment:Voriconazole 6/4 mg/kg body weight BID iv; meropenem 1g TID iv, and vancomycin 1g BID ivSwitched to caspofungin 70/50 mg iv QD (due to elevated liver enzymes)Changed to posaconazole 200 mg po QID (solution) lifelong therapy (to avoid liver toxicity). This was changed to posaconazole tablet formulation 300 mg QD po in the further course of the therapy after FDA and EMA approval.
Question 2: What treatment is recommended in the care of this patient?
Treatment: The Infectious Diseases Society of America Practice Guidelines for the Diagnosis and Management of Aspergillosis recommends voriconazole or lipid formulation of amphotericin B as first-line therapy.
Outcome: The mitral valve associated structure was resected in situ without further mitral valve reconstruction or replacement. Afterwards, patient stabilized and discharged for rehabilitation after several months of hospital stay.
Discussion: Fungal endocarditis is a rare disease accounting for only 2–4% of all cases of endocarditis. It occurs mostly in patients with predisposing host conditions. Well defined risk factors are intravenous drug use, indwelling catheters, prosthetic valves, pacemakers or joints, immunosuppression (solid organ/stem cell transplantation, chemotherapy and HIV), prolonged use of broad-spectrum antibiotics, and various chronic underlying diseases (e.g. diabetes mellitus and malnutrition) (1). Typically, Aspergillus endocarditis occurs after cardiac surgery, diverging from the case presented here. Clinical presentation of patients with fungal endocarditis is highly variable: unspecific symptoms vary from fever and dyspnea to pain in the chest and weakness (2).
Of utmost importance is early diagnosis followed by rapid surgical resection or debridement in combination with antifungal therapy. This is due to the high risk of cardiac decompensation and embolic complications. In case of fungal growth in culture, susceptibility testing is essential. The Infectious Diseases Society of America recommends voriconazole or liposomal amphotericin B as the preferred agents (3). We strongly advise therapeutic drug monitoring of voriconazole (3, 4). As recommended by the IDSA, lifelong antifungal therapy following surgical replacement of an infected valve is suggested.
Key References: (1) Ellis et al. Clin Infect Dis 2001 Fungal endocarditis: evidence in the world literature, 1965–1995.(2) Tacke et al. Curr Opin Infect Dis 2013 Fungal Endocarditis(3) Patterson et al. Clin Infect Dis 2016 Practice Guidelines for the Diagnosis and Management of Aspergillosis: 2016 Update by the Infectious Diseases Society of America (4) Ullmann et al. Clin Microbiol Infect. 2018 Diagnosis and management of Aspergillus diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline.
