Title: Rhinocerebral Mucormycosis
Submitted by: Dr. Mallika Devarapalli, Dr. Budder Siddiqui
Institution: Augusta University, Medical College of Georgia
Email: mdevarapalli@augusta.edu
Date Submitted: November 2, 2019
History:
This is a case of a 24-year-old old woman with a history of uncontrolled type I DM, diabetic retinopathy, numerous admissions for diabetic ketoacidosis, and a recent HbA1C at 11.4 who was admitted for increasing left sided facial swelling associated with associated tingling, numbness and severe pain. Additionally, she also reported to have lost vision in the left eye about 3 weeks ago prior to her presentation. Patient stated that her symptoms started about one month ago after an infected left upper tooth which was subsequently extracted by her local Dentist. Afterwards, she was placed on PO clindamycin, but her symptoms persisted despite completing her antibiotic therapy. She returned to her dentist 2 weeks later who removed all of her maxillary teeth and debrided the infection. The dentist noted that there was devitalized bone in the left maxillary sinus. He then advised the patient to be admitted to the hospital for this severe infection.
On admission, the patient had left facial swelling with no erythema, significant drooping of the left eyelid, facial asymmetry and an acute decline in her vision in her left eye. Oral cavity exam revealed black necrotic lesions on the left upper palate with associated edema (see Image 1A and B).


Physical examination:
Vitals: Temp: 36.9, HR: 104, RR:18, BP: 134/97, SpO2: 100%
General: No respiratory distress, wasted and acutely ill-appearing
Face: edema along the left side of the face extending to the mandible
Neck: supple, no lymphadenopathy
Pupils: dilated for eye exam, left lateral rectus palsy, poor visual acuity in L eye
Oral cavity: edentulous, black necrotic lesions on the left upper palate with swollen gums
Cardiac: regular rhythm, tachycardia without murmur
Pulmonary: CTA bilaterally, no use of accessory muscles, no audible wheezing
Abdomen: soft, non-tender, no organomegaly
Extremities: no edema, cyanosis, or clubbing
Neuro: numbness along the left V3 and tingling along left V1/V2; right V1-V3 sensation intact, no motor deficits
Labs:
WBC: 9.9
Hgb: 11.2
Na: 138
K+: 4.4
Cr: 0.46
Glucose: 138
Imaging
CT maxillofacial w/o contrast demonstrated significant bone demineralization and concern for Invasive Fungal Sinusitis (IFS) involving left nasal cavity, left orbital apex and floor, pterygoid, middle cranial fossa, and masticator space (see Image 2A and B).


Hospital Course
In view of a suspected IFI in a diabetic patient, and a high suspicion of Mucormycosis, liposomal amphotericin was initiated empirically, as well as IV ceftaroline and metronidazole to cover for possible superimposed bacterial sinusitis.
Pt was immediately taken to the OR for extensive debridement with functional endoscopic sinus surgery, medial maxillectomy, and pterygopalatine fossa (PPF) with the following findings:
- Necrotic tissue with purulent debris within the PPF
- Absent mucosa along the left posterior wall of the maxillary sinus with exposed and necrotic bone
- Purulent material within the left maxillary sinus floor
- Thrombosed ptergopalatine plexus and vessels
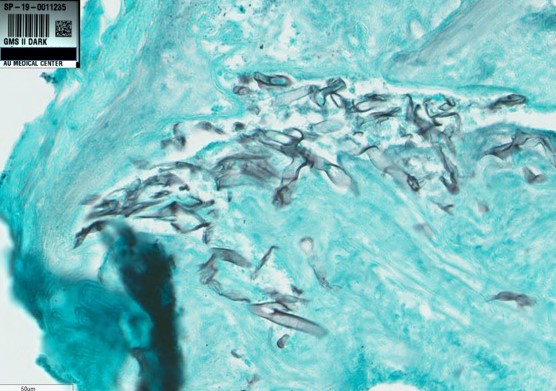
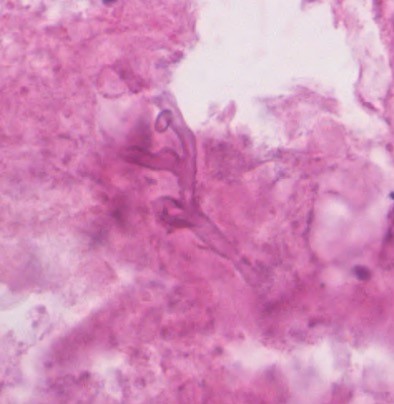
Frozen sections of the left maxillary sinus mucosa and left PPF contents taken intraoperatively reportedly showed aseptate fungal hyphae and necrotic tissue.
Microbiology:
Blood cultures: negative and final
Fungus culture: (left maxillary aspirate) – negative
Final Pathologic Diagnosis
Left maxillary sinus tissue consistent with IFI and left pterygopalatine fossa contents showed mostly necrotic tissue with rare fungal hyphae.
Diagnostic pathology comment: The organism resembled a Zygomycete
Treatment:
The patient was treated with IV liposomal amphotericin B and Isavuconazole dose in addition to aggressive control of her uncontrolled hyperglycemia.
Outcome:
-On day 10 of the hospitalization, patient had further debridement done with the following findings:
- necrotic infraorbital nerve and was removed
- coating of fibrinous exudate on PPF wall removed and debrided to healthy tissue.
- Necrotic tissue at the edge of the posterior aspect of the medial maxillary wall extending slightly into the ethmoid floor –was removed
Post operatively, the patient reported improved vision in left eye and improvement in left sided facial swelling/tingling/numbness.
Discussion:
Mucormycosis is usually a rare, fatal infection closely associated with uncontrolled diabetics. It is an opportunistic mold found in soil, rotten fruits/vegetables, and bread. It occurs via spore inhalation with angioinvasive dissemination. The literature describes several predisposing conditions associated with this infection such as lymphoma, leukemia, chemotherapy, severe burns but the most common condition is diabetes with ketoacidosis. Rapid fungal growth occurs in acidic environment secondary to increase glucose levels and free iron ion. It invades the walls of blood vessels causing rapid destruction involving all the structures in its path. More commonly, this infection invades ethmoid sinuses and eventually involves other structures such as the orbit and eye, bone and brain tissue extending into cavernous sinuses. According to the CDC, the mortality rate was 46% among those with sinus infections, 76% for those with pulmonary infections, and 96% for disseminated Mucormycosis. According to dental literature from 1958 to 1993, only 15 of 36 patients survived (42%), therefore early diagnosis is crucial in order to reduce mortality.
A high index of suspicion is necessary in order to initiate diagnostic and therapeutic modalities for Mucormycosis. Definitive diagnosis frequently requires a biopsy with histopathologic examination which is the most sensitive form of diagnosis. Unlike other fungi, Mucormycetes will appear as aseptate hyphal elements, ribbon-like, thick-walled that branch at right angles. Although cultures are positive in fewer than half of cases, Mucor may grow within 48 hours if laboratory is advised to cut the tissue into sections and place in the center of culture dishes rather than to homogenize the tissue.
In this patient, along with other cases of mucor, fungal cultures are negative and the histopathology was used to make the probable diagnosis of rhinocerebral mucormycosis. The key learning point in this case is that it is critical to suspect, diagnose and initiate antifungal therapy in order to improve morbidity and survival rates. Successful treatment of Mucormycosis requires four steps which include early suspected diagnosis, immediate and aggressive surgical debridement of infected tissue, followed by prompt appropriate antifungal therapy and reversal of underlying predisposing risk factor such as improved glucose control, recovery of neutropenia, hemochromatosis and eliminating or at least reducing any immunosuppressive agents.
Currently, recommended antifungal therapy includes either IV liposomal amphotericin B, followed by de-escalation to an oral azole such as isavuconazonium sulfate or posaconazole after clinical improvement. Unfortunately, the length of therapy is unknown, most clinicians will continue antifungal therapy until resolution of clinical signs and symptoms of infection and the reversal of underlying risk factors. Although repeat imaging to evaluate for resolution of disease is recommended, studies show greater emphasis should be placed on clinical response in the first 2-4 weeks after starting therapy rather than monitoring radiographic progression.
Key References:
- Kasper, Dennis L.,, et al. Harrison’s Principles of Internal Medicine. 19th edition. New York: McGraw Hill Education, 2015.
- Damante, J and Fleury, R. 1998. Oral and Rhinoorbital Mucormycosis. https://www.joms.org/article/S0278-2391(98)90883-7/pdf
- Mold Infections of the Central Nervous System. McCarthy M., Rosengart A., Schuetz A.N., Kontoyiannis D.P., and Walsh T.J.|N Engl J Med 2014; 371:150-160
- Rees JR, Pinner RW, Hajjeh RA, Brandt ME, Reingold AL. The epidemiological features of invasive mycotic infections in the San Francisco Bay area, 1992-1993: results of population-based laboratory active surveillance. Clin Infect Dis. 1998 Nov;27(5):1138-47.
- Chao, A and Kontoyiannis, D. Invasive Fungal Sinusitis in Immunocompromised Hosts. Infections of the Ears, Nose, Throat and Sinuses. 2018; 177-188
