Title: Rapidly Progressive Skin and Soft Tissue Infection
Submitted by Hutton Brandon MD, Folake Lawal MD, Cheryl Newman MD.
Institution: Medical College of Georgia at Augusta University
Email: flawal@augusta.edu
Date Submitted: 5/12/2020
History:
A 40-year-old man brought to the emergency department by the EMS with altered mental status of 4 days, hypothermia, an area of pain and swelling on his left hand. His mother reported that he had a spider bite on the dorsum of his left hand that became increasing swollen, red, and painful over the past four days. After missing several doses of insulin due to a shortage of injection needles, he started to experience generalized pain, polyuria, and polydipsia, prompting the visit to the emergency department. The patient was admitted for management of diabetic ketoacidosis in addition to possible sepsis and started on empiric antibiotic therapy with vancomycin and piperacillin-tazobactam.

PMH:
Insulin-dependent type II diabetes, methamphetamine abuse, Hepatitis B, right below knee amputation (BKA), Left above knee amputation (AKA), bipolar disorder
Physical Examination:
Vital Signs:
T: 35.7 °C, HR: 123bpm, RR: 13cpm, BP: 106/80 mmHg, SpO2: 100%
General: Patient was lethargic, cachectic, oriented to self and place.
Cardiovascular: Tachycardic, normal heart sounds, no murmurs.
Respiratory: Clear breath sounds on auscultation.
Musculoskeletal: Right below knee amputation, left above knee amputation.
Neurologic: Patient with altered mental status, unable to follow commands or answer questions appropriately.
Skin: Swelling and erythema with central eschar on dorsum of left hand, purulent drainage noted with peeling of surrounding skin.
Laboratory Examination:
CBC: WBC 21.6, Segs: 82%, ESR:116, Glucose: 588 mg/dL
Urine: Glu >1000, protein: 30, Ketones >80, Leukocyte esterase: negative.
Sodium: 145meq/L, K: 3.4 mEq/L, Cl:110 mEq/L, CO2: <10 mEq/L, Cr: 0.8mg/dlHIV screening: negative.
Question 1: What are probable/possible diagnoses?
This is most likely an abscess from Staphylococcus aureus or Streptococcal infection.
Microbiology/Diagnostic Tests Performed:
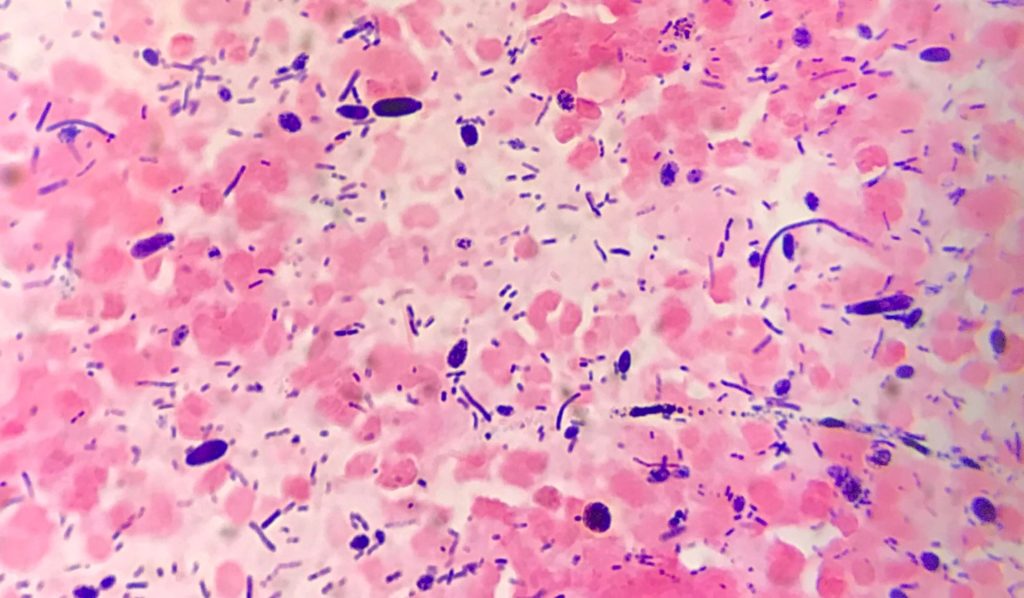
Bacterial and fungal cultures of the blood were negative. Gram stain and culture of wound swabs from incision and drainage in the operating room demonstrated 4+ yeast forms and 4+ Gram positive bacilli. The organisms were later identified as Candida tropicalis and Lactobacillus gasseri.
Final Diagnosis:
Polymicrobial Skin and soft tissue abscess due to C. tropicalis and L. gasseri.
Question 2: What treatment is recommended in the care of this patient?
Candida species have variable susceptibility to fluconazole but mostly susceptible to echinocandins. Micafungin is recommended empiric therapy prior to species identification. C. tropicalis has low rates of fluconazole resistance and it is an effective and convenient option to transition using high doses. Lactobacillus spp. are commonly resistant to vancomycin and may often be resistant to cephalosporins and quinolones as well. Penicillin, ampicillin, macrolides, or tetracycline can be used as treatment.
Treatment:
Micafungin was added to antimicrobial therapy following the results of the Gram stain and vancomycin discontinued in favor of ampicillin-sulbactam after identification of a Lactobacillus spp. He completed a course of oral fluconazole after discharge.
Outcome:
Upon further questioning after his mental status had recovered, the patient disclosed that the initial injury was not a spider bite but was the result of an unintentional subcutaneous injection of methamphetamine solution in a failed attempt to inject a vein on his hand. He was discharged after an 11-day hospital course that was complicated by Candida glabrata candidemia on day 6. The wound was healing well at follow-up two weeks after discharge and had healed completely at one month.
Discussion:
Candida tropicalis is a diploid yeast that is likely the 4th most common cause of Candida infection following Candida albicans. It is normally present on the skin, gastrointestinal, genitourinary, and respiratory tract. It has also been associated with a variety of both superficial and systemic infections, typically in patients who are neutropenic, have recently received antibiotics, or have damage to the gastrointestinal mucosa. It is uncommon as a cause of superficial infections such as oral candidiasis, vulvovaginal candidiasis, or onychomycosis. It is an extremely uncommon cause of skin or soft tissue infections such as cellulitis or abscess formation.
Lactobacillus spp. are gram positive facultative anaerobic, non-spore forming bacilli. They are rarely associated with infection but have been implicated in a variety of infections, associated with wound infections in intravenous drug users (IVDU).A large variety of organisms have been documented in skin/soft tissue infections in IVDU including many species of fungi. This is likely due to the use of unsterile equipment for injection, as well as the vasoconstrictive effects of injection drugs such as methamphetamine which can induce local skin necrosis. This necrosis possibly plays a role in the above case, providing ample culture media and allowing these pathogens to cause infection in an environment where they are normally not pathogenic.
Furthermore, the high blood glucose of this patient may also have played a role, inhibiting neutrophil function and allowing these organisms to spread. Polymicrobial infections with both fungal and bacterial species are well-document in diabetic foot infections.
The interactions between fungi and bacteria in these infections are still ill-defined. Many studies of vulvovaginal candidiasis have shown an antagonistic relationship between C. albicans and Lactobacillus spp., with lactobacillus inhibiting C. albicans growth and vice-versa. C. albicans can inhibit lactobacilli through the quorum-sensing compound farnesol. However, these mechanisms do not seem to have a played a significant role in the case of this patient as both organisms were quite abundant in the abscess.
IVDU caused traumatic inoculation in a person immunocompromised due to uncontrolled diabetes mellitus, the combination of these factors and co-infection with Lactobacillus gasseri and C. tropicalis two unusual causes of necrotizing infections culminated to this disease process. The co-infection may have had a synergistic activity leading to necrotic infection. Skin and soft tissue infections in immunocompromised patients should be treated with caution and investigated to identify specific etiology rather than empiric treatment in order to avoid extensive disease and systemic dissemination.
Key References:
- Del Giudice P. Cutaneous complications of intravenous drug abuse. The British journal of dermatology. 2004;150(1):1-10.
- Peleg AY, Hogan DA, Mylonakis E. Medically important bacterial-fungal interactions. Nature reviews Microbiology. 2010;8(5):340-349.
- Summanen P, Talan D, Strong C, et al. Bacteriology of skin and soft-tissue infections: comparison of infections in intravenous drug users and individuals with no history of intravenous drug use. 1995;20(Supplement_2):S279-S282.
- Zuza-Alves DL, Silva-Rocha WP, Chaves GM. An Update on Candida tropicalis Based on Basic and Clinical Approaches. Frontiers in microbiology. 2017; 8:1927.
- Tambot, Hennie G. MD*; Yu, Inski MD*; Cutrona, Anthony MD†‡§; Marnejon, Thomas DO*‡§ Lactobacillus gasseri: A Rare and Fatal Case of Fournier Gangrene in a Diabetic Woman, Infectious Diseases in Clinical Practice: March 2010 – Volume 18 – Issue 2 – p 132-134 doi: 10.1097/IPC.0b013e3181b9d31d
- Esquibel, A., Dababneh, A. S., & Palraj, B. R. (2017). Lactobacillus gassers Causing Bilateral Empyema. Case reports in infectious diseases, 2017, 4895619. https://doi.org/10.1155/2017/4895619
