Title: Heartbreak and Fungus: A Michigan Tale
Submitted by: Stephen Maurer, Shiwei Zhou, Carol Kauffman, Marisa Miceli
Institution: University of Michigan
Email: smaurer@med.umich.edu
History:
The patient is a 66-year-old man whose cardiac history includes a coronary artery bypass graft performed 20 years ago, a bioprosthetic aortic valve placed 10 years ago, an intra-cardiac defibrillator (ICD) inserted 7 years ago, and ischemic cardiomyopathy.
He was admitted in July with a 5-week history of debilitating fatigue, anorexia and eventually fevers as high as 38.3oC. During that time, he had been seen by his cardiologist, who discontinued amiodarone without any improvement in his symptoms. Elevated liver enzymes had been noted, and he underwent a liver biopsy that demonstrated granulomatous hepatitis with minimal periportal and sinusoidal fibrosis.
He had retired from his job as a county park superintendent in southeastern Michigan, but remained an active outdoorsman.
Physical Examination:
BP: 120/77, HR: 72, RR: 16, SpO2: 100% on room air, temperature 38.4oC
General: Well-appearing man in no distress
Cardiovascular: Regular rhythm, 2/6 systolic ejection murmur heard best at the right upper sternal border (unchanged from prior examinations), trace lower extremity edema.
Pulmonary: Clear to auscultation bilaterally with good air movement, normal work of breathing.
Abdomen: Soft, non-tender, no organomegaly.
Remainder of physical examination unremarkable.
Basic Laboratory Examination:
White Blood Cell Count: 5900/uL (Ref: 4000-10,000/uL)
Differential: 80% neutrophils, 10% lymphocytes, 8% monocytes
Hemoglobin: 11.3 g/dL (Ref: 13.5 – 17.0 g/dL)
Platelets: 132,000/uL (Ref: 150,000 – 400,000/uL)
Alanine aminotransferase: 137 IU/L (Ref: <35 IU/L)
Aspartate aminotransferase: 81 IU/L (Ref: 8 – 30 IU’L) Alkaline Phosphatase 171 IU/L (Ref: 30 – 116 IU/L)
Question 1: What are probable/possible diagnoses
Because of granulomatous hepatitis on liver biopsy and constellation of constitutional symptoms, initial differential diagnosis included systemic infection with:
- Histoplasma capsulatum
- Blastomyces dermatitidis
- Brucella spp.
- Coxiella burnetii
- Mycobacterium tuberculosis
Non-infectious differential diagnosis included:
- Sarcoidosis
- Primary biliary cholangitis
- Drug toxicity (i.e., amiodarone)
- Idiopathic granulomatous hepatitis
Microbiology/Diagnostic Tests Performed:
– Computed tomography (CT) Chest/Abdomen/Pelvis: Areas of low attenuation within the spleen with possible splenic infarct
– Fungal Serology: H. capsulatum complement fixation antibody 1:512 (mycelial phase); 1:512 (yeast phase); immunodiffusion H and M bands present
– Serum Histoplasma antigen by enzyme immunoassay: 1.98 ng/mL
– Urine Histoplasma antigen by enzyme immunoassay: 1.69 ng/mL
– Culture of blood using lysis centrifugation technique: By day 9, growth of a mold was noted on the Sabouraud dextrose agar plate incubated at 30oC; identification by DNA probe verified that the organism was H. capsulatum
– Transesophageal echocardiogram (TEE) showed a large mobile echodensity (18mm x 10mm) on the non-coronary cusp of the bioprosthetic aortic valve concerning for vegetation with possible peri-prosthetic abscess (figure 1A) as well as thickening of mid and tip of anterior leaflet of the mitral valve with small mobile echo densities suspicious for vegetation (figure 1B)
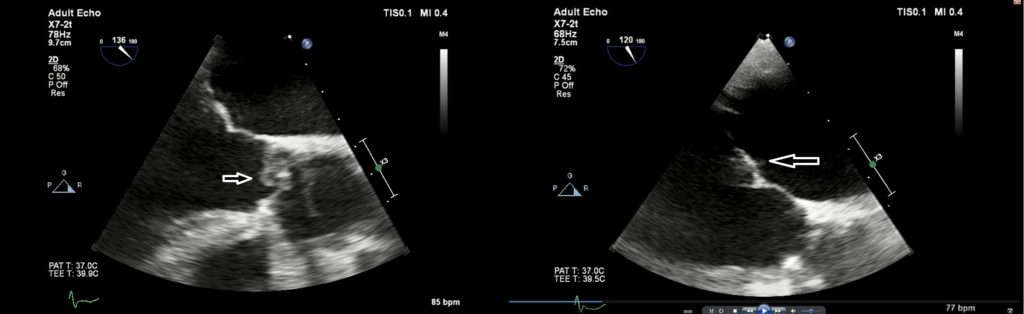
Figure 1B: TEE image of native mitral valve with thickening of mid and tip of anterior leaflet with small mobile echodensities (ARROW) suspicious for vegetations
He underwent aortic valve replacement, aortic root reconstruction, removal of the ICD, and
mitral valve repair.
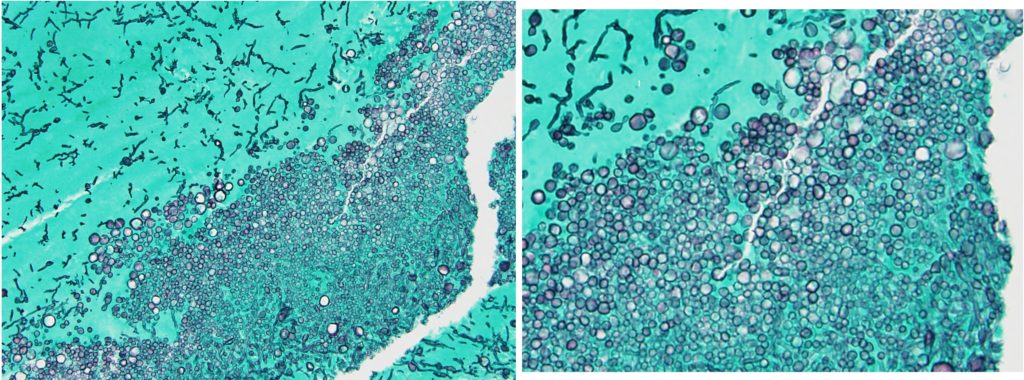
– Histopathology of aortic valve tissue showed both yeast-like structures of various sizes and hyphae (figure 2)
Final Diagnosis: H. capsulatum endocarditis of bioprosthetic aortic valve and native mitral valve
Question 2: What treatment is recommended in the care of this patient?
For severe disseminated histoplasmosis, the IDSA guidelines for management of histoplasmosis recommend treatment with 3 mg/kg daily of liposomal amphotericin B with alternatives of 5 mg/kg/day of another lipid formulation or 0.7-1mg/kg/day of amphotericin B deoxycholate for 1-2 weeks, followed by oral itraconazole for at least 12 months. Itraconazole may be required as lifelong therapy for immunosuppressed patients or patients who relapse despite appropriate therapy [1].
The guidelines do not specifically comment on management of Histoplasma endocarditis, but in most case series in addition to antifungal therapy, surgery is essential to decrease organism burden and to improve valvular function. Only one patient in two case series comprising a total of 19 patients survived without surgical management [2,3].
Treatment and Outcome:
This patient was treated with liposomal amphotericin B 5 mg/kg IV daily. He underwent replacement of the bioprosthetic aortic valve, aortic root replacement, mitral valve repair, and extraction of the ICD.
His postoperative course was complicated by both septic and cardiogenic shock. After seven weeks of treatment with IV liposomal amphotericin B, treatment was changed to oral itraconazole, 200 mg twice daily after a 3-day loading dose. He continued to decline and ultimately decided on comfort care and died shortly thereafter.
Discussion:
H. capsulatum is a dimorphic fungus most commonly seen in North and Central America. In the United States, it is considered endemic in the Mississippi and Ohio River valleys, which includes Michigan, where this patient lived [4].
The primary reservoir of H. capsulatum is soil, particularly that containing large amounts of bird or bat guano [4]. Infection results from inhalation of Histoplasma microconidia, often in the setting of environmental disturbances [5]. As a retired superintendent of the county park system, our patient worked outdoors and continued to spend a large amount of time outdoors in retirement.
Histoplasma infection is typically asymptomatic, or characterized by self-limited mild illness never identified as being histoplasmosis. It is estimated that <1% of patients develop symptomatic disease [4].
Histoplasmosis manifests most commonly as an isolated pulmonary infection, with both acute and chronic presentations being described. Disseminated histoplasmosis is less common, and found more in immunosuppressed hosts (i.e. those with HIV/AIDS, solid organ or hematopoietic cell transplant, hematologic malignancies, treatment with corticosteroids or tumor necrosis factor inhibitors). A chronic progressive form of disseminated histoplasmosis is seen mostly in older adults who have no obvious immunosuppression.
Histoplasma endocarditis is an uncommon manifestation of histoplasmosis. It may present as isolated valvular infection, but in as many as 70% of patients, cardiac involvement is only one manifestation of disseminated disease [6]. Blood cultures often yield no growth, or the organisms grow only after several weeks; thus, Histoplasma endocarditis should always be included in the differential diagnosis of culture-negative endocarditis [2]
Liposomal amphotericin B is the drug of choice for initial treatment of severe infections, including endocarditis, and has been noted to clear fungemia more quickly than azoles [7]. Initial treatment for several weeks is typically followed by oral itraconazole. The timing of this transition depends on the patient’s response to initial therapy [1].
Our patient’s presentation is consistent with the risk group most commonly noted in one multicenter review of 14 patients with Histoplasma endocarditis, in which 10 of 14 cases were men with infected prosthetic aortic valves. In this review, symptoms were present for a median of 7 weeks before diagnosis. The most useful laboratory tests were urine and serum Histoplasma antigen assays [3].
In the above-noted series, surgical management was required in 11 of the 14 patients. Almost all patients received IV amphotericin B as initial therapy (median = 29 days) followed by itraconazole. Duration of suppressive therapy varied from 11 months to lifelong. The 3 deaths in this series were in patients who had received no or minimal amphotericin B [3].
In another case series of 5 patients, 3 were men, the median age was 62 years, and all had involvement of prosthetic endovascular material. Four of the 5 patients responded to combined medical/surgical treatment [2].
In summary, we present a case of Histoplasma endocarditis on a prosthetic aortic and native mitral valve. Unfortunately, our patient had a fatal outcome despite appropriate treatment with intravenous liposomal amphotericin B and cardiac surgery.
Key References:
1. L. Joseph Wheat, Alison G. Freifeld, Martin B. Kleiman, John W. Baddley, David S. McKinsey, James E. Loyd, Carol A. Kauffman, Clinical Practice Guidelines for the Management of Patients with Histoplasmosis: 2007 Update by the Infectious Diseases Society of America, Clinical Infectious Diseases, Volume 45, Issue 7, 1 October 2007, Pages 807–825, https://doi.org/10.1086/521259
2. Ledtke C, Rehm SJ, Fraser TG, Sretha NK et al. Endovascular infections caused by Histoplasma capsulatum: a case series and review of the literature. Arch Pathol Lab Med. 2012;136(6):640-5. PMID: 22646271
3. Riddell J 4th, Kauffman CA, Smith JA, Assi M et al. Histoplasma capsulatum endocarditis: multicenter case series with review of current diagnostic techniques and treatment. Medicine (Baltimore). 2014;93(5):186-93. PMID:25181311
4. Kauffman CA. Histoplasmosis: a clinical and laboratory update. Clin Microbiol Rev. 2007 Jan;20(1):115-32. doi: 10.1128/CMR.00027-06. Review. PubMed PMID: 17223625; PubMed Central PMCID: PMC1797635
5. Benedict K, Mody RK. Epidemiology of Histoplasmosis Outbreaks, United States, 1938-2013. Emerg Infect Dis. 2016 Mar;22(3):370-8. doi: 10.3201/eid2203.151117. PMID: 26890817; PMCID: PMC4766901
6. Antinori S, Ferraris L, Orlando G, Tocalli L, et al. Fungal endocarditis observed over an 8-year period and a review of the literature. Mycopathologia. 2014;178(1-2):37-51. PMID24965217
7. Wheat LJ, Cloud G, Johnson PC, Connolly P, Goldman M, Le Monte A, Fuller DE, Davis TE, Hafner R. Clearance of fungal burden during treatment of disseminated histoplasmosis with liposomal amphotericin B versus itraconazole. Antimicrob Agents Chemother. 2001 Aug;45(8):2354-7. doi: 10.1128/AAC.45.8.2354-2357.2001. PubMed PMID: 11451696; PubMed Central PMCID: PMC90653
