Progressive visual field loss, confusion, headache for 2 months
Authors:
Peter G. Pappas,
- 64 yo black male with recent onset of progressive visual loss on R visual field, confusion and headache. Symptoms have progressed over 2 months
- Until then the patient was in his usual state of health, no recent hospitalizations, procedures or history of trauma.
- Otherwise the patient denies fever, seizures, paresthesias, paresis, vertigo, or falls.
- Has a history of Evans Syndrome for which he takes low dose prednisone daily (10-20 mg/d)
PMH:
- HTN
- Evan’s Syndrome
- Meds: Prednisone, Lisinopril, albuterol, HCTZ
- Social: From Birmingham, AL, no travel hx, no pets, denies ETOH, tobacco, drugs
- Occupation- Physical Therapist- at a local hospital
Physical Examination:
- VS: BP 135/80 HR 75 Temp 36.9
- General: Alert and oriented.
- HEENT: PERRLA, EOMI. No oral lesions
- Neck: Supple, no LAD.
- Lungs are clear to auscultation.
- CV: RRR, no MGR.
- Abd: soft, NT, ND. No VCM.
- Neurologic: R homonymous hemianopsia, normal sensory, 5/5 strength and normal sensory. Up-going toes on L foot. No clonus. 2+ LE reflexes.
Laboratory Examination:
- WBC 8.95
- Diff: Neu 71/ Ly 16/ Mo 8/ Eo 4
- H/H 12 gms/36%
- PTL 123K
- BMP wnl
- CXR wnl
- HIV neg
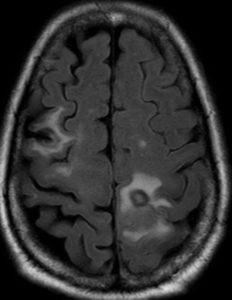
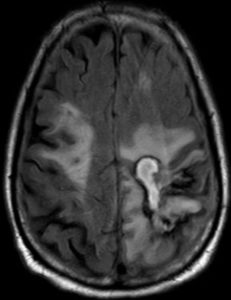
Imaging: MRI- March 2016
(MRI-1)
Hospital course:
- Left parietal craniotomy and partial resection of abscess
“The abscess was gray in color and chalky in consistency. It was removed by establishing margins.”
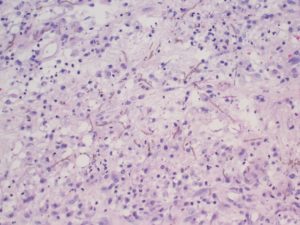
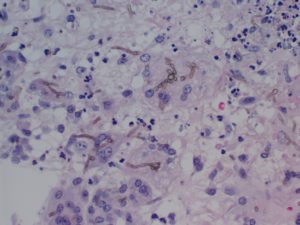
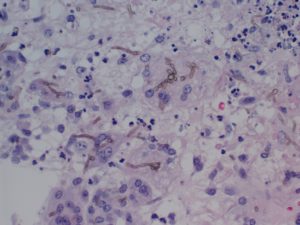
Pathology: Brain Biopsy (Histology 1, 2, 3, 4)

Question: What is your diagnosis?
Microbiology:
- GS: fungal elements 2+
- Culture:
- Abundant Cladophialophora bantiana
- Amphotericin B = 0.5
- Posaconazole = 0.125
- Voriconazole = 1
- Abundant Cladophialophora bantiana

(MICRO1)
Diagnosis: Cerebral Phaeohyphomycosis; Species: Cladophialophora bantiana
Clinical Course:
Medical management:
- Ampho B, voriconazole, decadron, phenytoin started after brain biopsy.
- Improved slowly over 2 weeks, then transferred to rehab facility
Discussion:
Phaeohyphomycosis
- Dematiaceous fungi (melanin-like pigments)
- Phaeo is Greek for “dark”.
- Variety of infections in humans
- Subcutaneous, deep soft tissue
- Invasive
- Brain abscess
Nomenclature:
- Cerebral phaeohyphomycosis:
- Most common:
- Cladosporium trichoides
- Xylohypha bantiana
- Cladosporium bantianum
- Cladophialophora bantiana
- Other causative fungi:
- Wangiella dermatitidis (Exophiala dermatitidis)
- Dactylaria gallopava (Ochroconis gallopava)
- Fonsecaea pedrosoi,
- Bipolaris spicifera (Drechslera spicifera), Rhinocladiella mackenziei (Ramichloridium mackenziei and Ramichloridium obovoideum) and Aureobasidium species.
- Most common:
Pathogenesis of CNS Disease:
- Extension from the adjacent paranasal sinuses
- Inhalation and proliferation of spores
- Directly from penetrating trauma to the head
- Hematogenous dissemination
- Localized skin lesions
- Injection drug use
- Heart-lung transplant patient with pneumonitis
Epidemiology/Clinical Features:
- Half of the cases had no apparent immunossupression (Clin Infect Dis. 2004;38(2):206)
- Cases present with focal neurologic deficits and/or generalized seizures.
- Fever and headache are uncommon.
- Symptomatic sinusitis or localized infection due to dematiaceous fungi at another site is very rare.
- Meningeal involvement is unusual.
Diagnosis and Treatment:
- Microscopic examination
- Branching, brown septate hyphae on H&E or KOH
- Rarely, the hyphae do not have pigment
- Special stains for melanin (Fontana-Masson stain)
- Grow relatively quickly from clinical specimens.
- Identification is based on morphology of cultures
- Reference laboratories
- Surgical resection + antifungals
- Susceptibly cut offs are not standardized
- Voriconazole, posaconazole, amphotericin B
Outcomes:
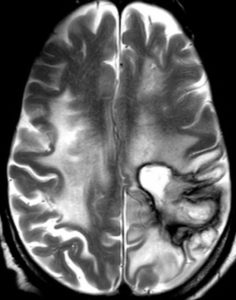
In March 2017, worsening CNS symptoms while taking voriconazole. Pt. was switched to posaconazole 300 mg/d
(Brain MRI 2)
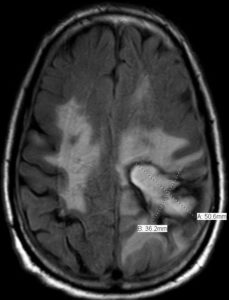
Despite posaconazole therapy, patient developed progressive symptoms. Repeat biopsy was performed due to progressive symptoms and for decompression, debulking of the lesion.
(Brain MRI 3)
| 10/8/2017 | Cladophialophora bantana |
| Drug | FDIL |
| 5-Flurocytosine | 0.25 |
| Amphotericin-B | 1 |
| Itraconazole | </= 0.03 |
| Posaconazole | <= 0.03 |
| Voriconazole | 0.125 |
Cladophilalophora bantana
- Terbinafine 0.03 ug/ml
- Isavuconazole 0.125 ug/ml
Ultimately patient switched to isavuconazole, flucytosine, and terbinafine. Symptoms progressed; patient died February 2018.
(Brain MRI 4)
References:
Revankar SG. Cladophialophora bantiana brain abscess in an immunocompetent patient. The Canadian Journal of Infectious Diseases & Medical Microbiology. 2011;22(4):149-150.
M.E. Brandt & D.W. Warnock (2013) Epidemiology, Clinical Manifestations, and Therapy of Infections Caused by Dematiaceous Fungi, Journal of Chemotherapy,15:sup2, 36-47, DOI: 10.1179/joc.2003.15.Supplement-2.36
Sutton DA, Slifkin M, Yakulis R, Rinaldi MG. U.S. Case Report of Cerebral Phaeohyphomycosis Caused by Ramichloridium obovoideum (R. mackenziei): Criteria for Identification, Therapy, and Review of Other Known Dematiaceous Neurotropic Taxa. Journal of Clinical Microbiology. 1998;36(3):708-715.
