History:
35yr old male with a past medical history of hemophilia A and IgA nephropathy complicated by end stage renal disease on peritoneal dialysis status post failed deceased donor kidney transplant presented to the emergency room with diffuse and sharp abdominal pain. The patient was in his usual state of health until three days prior to admission when he developed abdominal pain surrounding his peritoneal dialysis catheter site. His pain progressed in severity and was associated with significant nausea and “cloudy” catheter effluent. He states he has had chronic pruritus surrounding the catheter site and frequently attempts to scratch this area.
Physical Examination:
Temp: 36.1 °C (97 °F) | BP: 127/87 mmHg Pulse: 117 | Resp: 17 | SpO2: 99 % | Flow (L/min): 2 Weight: 66.7 kg (147 lb 0.8 oz)
- General Appearance: alert, non-toxic appearing, in no distress, but endorsing throat pain so unable/unwilling to speak
- Eyes: conjunctivae and corneas clear. PERRL, EOM’s intact, sclera normal.
- Mouth: oropharynx clear.
- Heart: S1/S2 regular, no murmurs.
- Lungs: clear to auscultation bilaterally.
- Abdomen: abdomen with multiple post-operative and well-healed scars; bandage over LLQ where Peritoneal dialysis catheter had been removed. No areas of surrounding skin breakdown, or erythema or induration. Abdomen exhibited diffuse tenderness and mild rebound and guarding.
- Extremities: no edema
- Skin: no rashes, lesions.
- Mental Status: alert and fully oriented.
- Musculoskeletal: no joint swelling.
Laboratory Examination: CBC:
WBC 17.2, H/H 9.2, Plts 297 CMP: Na 135, K 3.8, Cl 90, CO2 29, BUN 39, Cr 12.16, Gluc 102 LFTs: AST 33, ALT 37, ALP 134, ALB 3.1, TP 8.2, TBIL 0.3
Cultures were obtained from his peritoneal fluid and he was empirically started on ceftazidime and vancomycin.
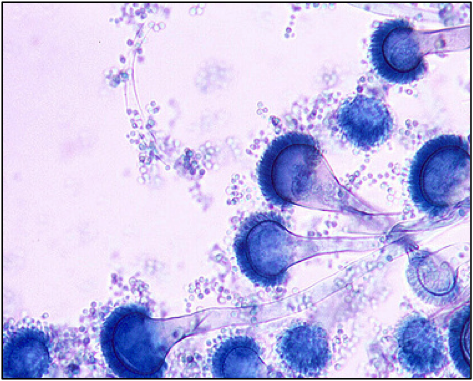 The day following admission his effluent cultures grew a mold (Figure 1) and he was transferred to a nearby tertiary care facility.
The day following admission his effluent cultures grew a mold (Figure 1) and he was transferred to a nearby tertiary care facility.
Diagnosis:
Aspergillus fumigatus peritonitis.
Question:
What treatment is recommended in the care of this patient?
Discussion:
Prompt peritoneal dialysis catheter removal accompanied by systemic antifungal therapy with voriconazole is currently recommended.
Aspergillus peritonitis may occur as a complication of chronic ambulatory peritoneal dialysis (PD) (1). Although Candida species are the most common cause of fungal peritonitis complicating chronic ambulatory peritoneal dialysis and typically occurs following an episode of bacterial peritonitis, Aspergillus species are an additional cause of this infection. The diagnosis can be suggested by detection of (1?3)-?-D-glucan and GM in the peritoneal fluid, or confirmed by culture of peritoneal fluid (2). In rare cases peritoneal biopsy is required although this is typically accomplished concurrently with PD catheter removal.
Removal of the dialysis catheter is essential in cases of fungal peritonitis and has been associated with improved survival. In cases where the catheter cannot be promptly removed, some practitioners use intraperitoneal amphotericin B in conjunction with voriconazole, but it should be recognized that intraperitoneal AmB administration may cause a chemical peritonitis and is not recommended by most experts (3). With rare exception, the catheter should be immediately removed.
Following catheter removal systemic antifungal therapy is required. Intravenous amphotericin B formulations result in suboptimal and in many cases undetectable peritoneal drug concentrations. Systemic therapy with voriconazole for 6-8 weeks is thus recommended based upon successful reports and adequate peritoneal concentrations in conjunction with catheter removal. Posaconazole and the echinocandins have been successfully used in fungal peritonitis from other causes and may have utility as salvage therapy in Aspergillus peritonitis. No data regarding isavuconazole for the treatment of peritonitis is yet available. Following treatment, a minority of patients may successfully return to peritoneal dialysis.
Key References:
- Nannini EC, Paphitou NI, Ostrosky-Zeichner L. Peritonitis due to Aspergillus and zygomycetes in patients undergoing peritoneal dialysis: report of 2 cases and review of the literature. Diagn Microbiol Infect Dis. 2003 May;46(1):49-54.
- Ates O, Metan G, Dundar T, Kiziltepe M, Kocyigit I, Unal A, et al. Diagnosis of Aspergillus niger peritonitis in a peritoneal dialysis patient by peritoneal galactomannan and beta-D-glucan detection. Perit Dial Int. 2013 Mar-Apr;33(2):216-8.
- Matuszkiewicz-Rowinska J. Update on fungal peritonitis and its treatment. Perit Dial Int. 2009 Feb;29 Suppl 2:S161-5.
