Synonyms
North American histoplasmosis. Contrast with African histoplasmosis due to Histoplasma duboisii
Definition
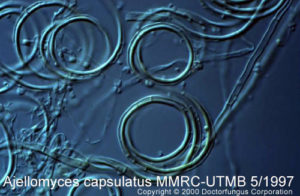
Histoplasmosis refers to the condition caused by the infection with the dimorphic endemic fungi N/A(L):Histoplasma capsulatum var. capsulatum. This anamorphic fungus has a known sexual teleomorph that carries the name Ajellomyces capsulatus. The majority of acute cases of infection with this fungus follow a subclinical and benign course in normal hosts [2412]. However, a disseminated and potentially fatal picture is seen among immunosuppressed individuals, children less than 2 years old, elderly persons, and people exposed to very large inoculum [872]. Since the advent of the HIV epidemic, histoplasmosis has reemerged to become one of the most frequent opportunistic diseases in those areas of the world endemic for this soil-based fungus [2031, 2418]. The infection is acquired through inhalation of Histoplasma capsulatum microconidia. The lungs are thus the most frequently affected site and chronic pulmonary disease may occur. This clinical picture is frequently associated with preexisting chronic lung diseases such as emphysema and occurs most frequently in elderly men [871]. All stages of this disease may mimic tuberculosis. Histoplasmosis may coexist with actinomycosis, other mycoses, sarcoidosis, or tuberculosis [1823, 1838].
Forms of the disease
| CATEGORIES | NOTES |
|---|---|
| Asymptomatic |
|
| Acute & symptomatic | |
| 1.- Self-limited (Flu-like syndrome) |
|
| 2.- Acute Pulmonary |
|
| 3.- Acute Pericarditis |
|
| 4.- Rheumatologic manifestations |
|
| Chronic Pulmonary |
|
| Disseminated |
|
| Fibrosing Mediastinitis |
|
Adapted from [2412]
DISSEMINATED HISTOPLASMOSIS: CLINICAL PRESENTATIONS
| ORGAN INVOLVED | CLINICAL MANIFESTATION |
|---|---|
| Lymph nodes |
|
| Bone Marrow |
|
| Heart |
|
| Adrenal glands |
|
| CNS |
|
| GI tract |
|
| Eyes |
|
| Skin |
|
| Genitourinary tract |
|
Prognosis and therapy
Special resource: You may also want to refer to the Infectious Disease Society of America-Mycoses Study Group (IDSA-MSG) Practice Guidelines for this disease. It is available at the (E):IDSA website.
Not all clinical manifestations require antifungal treatment. As mentioned above, there are self-limited pictures as well as inflammatory reactions that do not respond to specific antifungal agents. A panel of experts recently met and created a detailed set of guidelines for the treatment of histoplasmosis and the following table summarizes their recommendations [2415]:
| CATEGORIES | ANTIFUNGAL TREATMENT | REGIMEN |
|---|---|---|
| Asymptomatic | Not indicated | |
| Acute & symptomatic | ||
| 1.- Self-limited (Flu-like syndrome) | Not indicated | |
| 2.- Acute Pulmonary | Treatment indicated ONLY IF presents with hypoxemia or lasts for >1 month | Amphotericin B +/- corticosteroids1, follow by Itraconazole for a total of 6-12 weeks of therapy |
| 3.- Acute Pericarditis | Not indicated | Nonsteroidal anti-inflammatory agents for 2-12 weeks. Some may want to use corticosteroids for severe cases, in which case antifungal therapy is recommended |
| 4.- Rheumatologic manifestations | Not indicated | Nonsteroidal anti-inflammatory agents |
| Chronic Pulmonary | Treatment indicated | Amphotericin B followed by Itraconazole for a total of 12-24 months |
| Disseminated in non-AIDS | Treatment indicated | Amphotericin B followed by Itraconazole2 for a total of 12 weeks |
| Disseminated in AIDS | Treatment for life | Amphotericin B followed by Itraconazole2,3 for life |
| Fibrosis Mediastinitis | Controversial. To be considered in cases with elevated ESR or complement fixation titers >1:32 | Itraconazole for 3 months |
1The use of corticosteroids is controversial
2Ketoconazole can also be used although is less well tolerated than itraconazole.
3Fluconazole can also be used although has less efficacy than itraconazole.
Histopathology
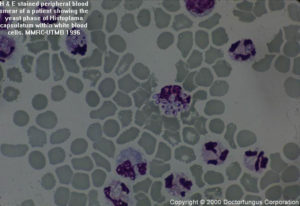
The histopathological picture in acute disseminated histoplasmosis is different from that seen in the more chronic disease, and in solitary pulmonary nodules (“coin lesion”). In the first entity, the organisms are localized in histiocytes and reticuloendothelial cells. The cells enlarge, but with no evidence of inflammation. The intracellular budding yeasts are approximately 3 µm in diameter, similar to Leishmania sp., but do not contain a kinetoplast. In addition, Leishmania does not stain with the special stains used for fungi. Older lesions show well-developed granulomata and have a central area of caseation resembling tuberculosis. The solitary pulmonary nodules are well organized and usually have a circumferential rim of calcification accounting for their visibility on chest X-ray. Fungi within these nodules are usually dead. Histoplasma capsulatum yeast are found in the center of the lesions.
Laboratory
Direct examination
The direct detection of fungi in clinical material such as bone marrow, sputum, and tissue is usually difficult. Material stained by the PAS, Giemsa, GMS or cellufluor methods is more likely to show the organisms than is a KOH preparation.
Isolation
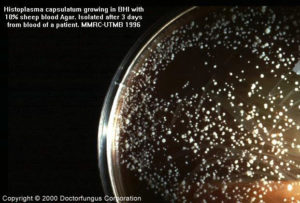
Inoculate the clinical material onto Inhibitory Mould agar and/or yeast extract-phosphate agar and/or BHI agar with 10% sheep blood and/or a medium containing cycloheximide. Incubate cultures at 30°C and do not discard until 12 weeks.
Antigen detection
Detection of the capsular antigen of this fungus in urine or serum is a very powerful tool for the diagnosis of the disseminated forms of this disease [333, 749, 2417, 2419]. The test is useful for both diagnosis and monitoring of infection, and is available from the (E):Histoplasmosis Reference Laboratory.
Laboratory confirmation
Confirmation is necessary to ensure that the fungus is not a species of Chrysosporium or Sepedonium. This can be accomplished by mould-to-yeast conversion, exoantigen testing, or by use of DNA probes.
Susceptibility testing
Standardized testing procedures are not available. Microbiological resistance has been demonstrated with respect to fluconazole [2413], but not itraconazole. Susceptibility testing is not routinely used to guide therapy of this disease.
Related sites and useful links
- The (E):Histoplasmosis Reference Laboratory has useful information on both their antigen detection test and on histoplasmosis in general. This site also provides a useful (E):map of the endemic regions for histoplasmosis.
- NIOSH provides a page on (E):protection of workers at risk for exposure to histoplasmosis.
- (E):EnviroHisto is a company specializing in environmental histoplasmosis issues.