Synonyms
Fungal ear infection, mycotic otitis externa
Definition
Otomycosis is a superficial mycotic infection of the outer ear canal. The infection may be either subacute or acute and is characterized by inflammation, pruritus, scaling, and severe discomfort. The mycosis results in inflammation, superficial epithelial exfoliation, masses of debris containing hyphae, suppuration, and pain and is responsible for ~9% of outer ear infections [1].
Risk Factors
- Residence in subtropical and tropical locations (likely due to higher humidity)
- Immunodeficiency (eg diabetes mellitus)
- Swimming
- Frequent manipulation of ear canal (scratching, cleaning, etc)
Diagnosis
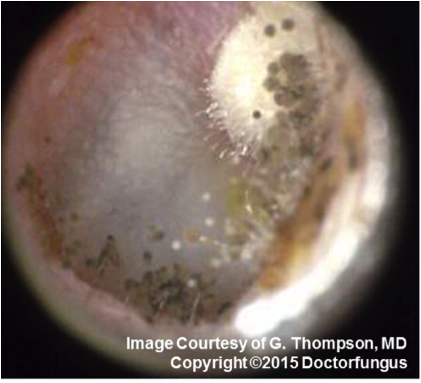
Direct examination of the auditory canal with an otoscope is revealing for fungal elements and spores, and findings are more frequent in the medial aspect of the ear canal.
Prognosis and therapy
Otomycosis may be a chronic recurring mycosis and correction or improving control of underlying immunodeficiency and keeping the ear canal dry are paramount in management (eg diabetes control). Cleaning or debridement of the auditory canal is essential using a cerumen loop or cotton swab (ENT referral may be necessary). Topical antifungals with proven efficacy include clotrimazole 1% solution (twice daily for 10-14 days), miconazole, nystatin, and econazole [2, 3].
Burrow’s solution or 5% aluminum acetate solution, aqueous solution of 0.02-0.1% phenyl mercuric acetate, 1% thymol in metacresyl acetate, or iodochlorohyroxyquin have all been used historically.
Histopathology
Inflammatory response with hyphae in the epithelium and in the exudate.
Laboratory
Direct examination
Epithelial debris placed in 10% KOH should reveal the presence of hyphae or yeast and in some instances the fruiting structures of the etiologic agent.
Isolation
The clinical material should be inoculated onto Sabouraud dextrose agar, IMA and incubated at 30°C. Since most of the fungi that cause this infection are sensitive to cycloheximide, a medium with cycloheximide has little value. Additional media containing antibacterial agents may be helpful if there is a heavy bacterial growth in the clinical material.
Mycology (principal fungi)
Aspergillus niger
Aspergillus fumigatus
Candida albicans
Candida tropicalis
References
- Munguia R, Daniel SJ. Ototopical antifungals and otomycosis: a review. Int J Pediatr Otorhinolaryngol 2008; 72(4): 453-9. PMID: 18279975
- Vennewald I, Klemm E. Otomycosis: Diagnosis and treatment. Clin Dermatol 2010; 28(2): 202-11. PMID: 20347664
- Ho T, Vrabec JT, Yoo D, Coker NJ. Otomycosis: clinical features and treatment implications. Otolaryngol Head Neck Surg 2006; 135(5): 787-91. PMID: 17071313