Synonyms
Tinea alba, tinea versicolor, tinea flava, achromia parasitica, dermatomycosis furfuracea
Definition
Pityriasis versicolor is a mild to chronic colonization of the stratum corneum by the lipophilic fungi N/A(L):Malassezia furfur. It causes characteristic discolored or depigmented lesions of the skin.
Epidemiology
Pityriasis versicolor is classically a disease affecting young people around the pubertal time probably related with hormonal changes and increase in sebum secretion. However, children are not excluded from suffering this fungal infection [2231]. Both males and females can be equally affected.
High temperatures and humidity favor the occurrence of pityriasis versicolor. Accordingly, tropical areas can have a prevalence as high as 40% and the frequency is higher during summer months in temperate climates [2199].
Clinical manifestations
Multiple macules and/or patches of variable appearance (hypopigmented, hyperpigmented, dark brown or erythematous) surrounded by normal skin are the typical lesions of pityriasis versicolor. The extension and severity of the lesions tend to be worse in tropical climates [701]. Affected areas include the back, chest, abdomen, neck, and upper limbs. However, classically the back carries more lesions. The face is an area commonly affected in children and it is the forehead showing mostly hypopigmented macules that is found [2230, 2231]. Uncommon but possible locations include axilla, popliteal fossa, forearms, lower limbs, radiotherapy field and penis/genitalia [2199].
Diagnosis
The diagnosis is usually based on clinical grounds. Nevertheless a useful, rapid and easy way to confirm the diagnosis is by using a Wood’s lamp. Yellow to yellow-green fluorescence is characteristic of fine scales taken from actvie lesions. Although the sensitivity of this procedure is reduced when patients have taken a recent shower [2199].
Prognosis and therapy
Therapeutic options include the use of topical agents and oral medication. Topical therapy is cheaper and probably safer, however compliance is sometimes low because of odor, difficulties in applying the solution to the back and/or the length of time the solution must be kept on. Topical agents include selenium sulfide shampoo, zinc pyrithione shampoo, ciclopirox olamine, propylene glycol lotions, topical terbinafine, and benzoyl peroxide [615, 2314]. Lotions are left on for about 10 minutes and then washed off. This treatment is repeated daily for 7 days and then once a month for 6 months.
Systemic therapy with either ketoconazole, fluconazole, and itraconazole are alternatives for patients not responding to topical therapy, frequent relapses or severe disease [561, 1564, 2484]. Oral terbinafine is not effective, probably because required fungicidal levels for N/A(L):Malassezia furfur are too high to be reached on the stratum corneum [138].
Mycology
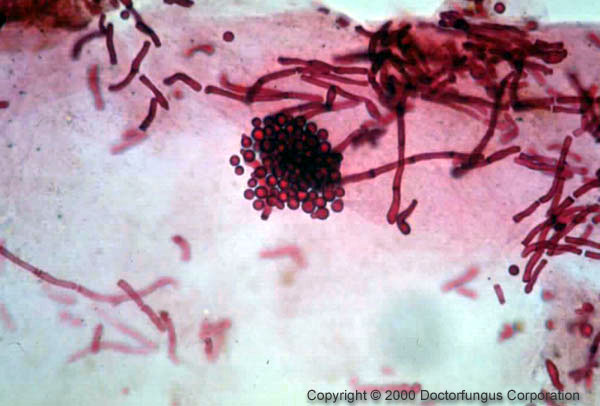
N/A(L):Malassezia furfur is not usually cultured since it is lipophilic. It can be cultured by adding olive oil to the isolation medium. The yeast will grow in 3-7 days at 30°C. The yeast has also been isolated from blood cultures of neonates undergoing parenteral nutrition and from persons with IV catheters.
Natural habitat
Humans