Case #3 – COVID-19 and Aspergillosis
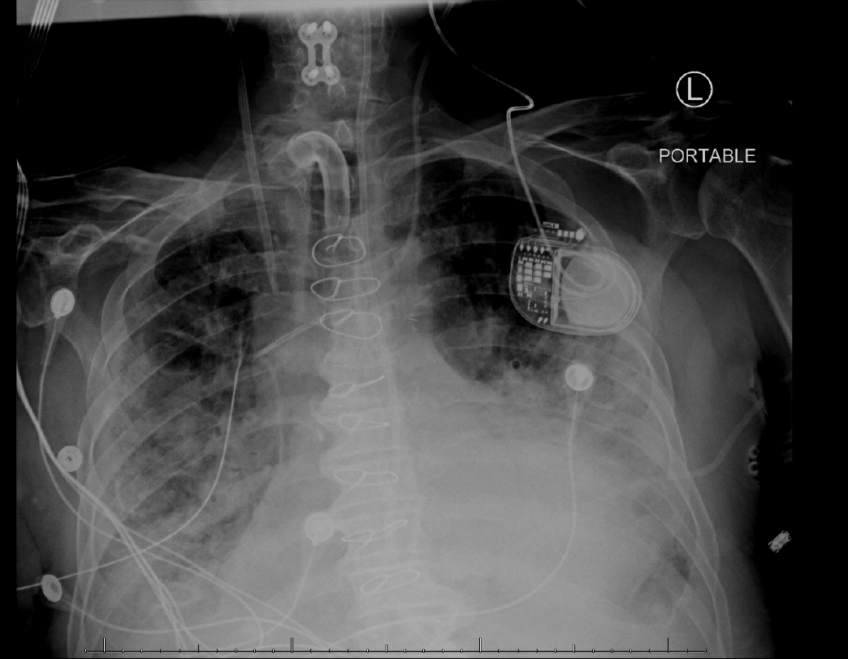
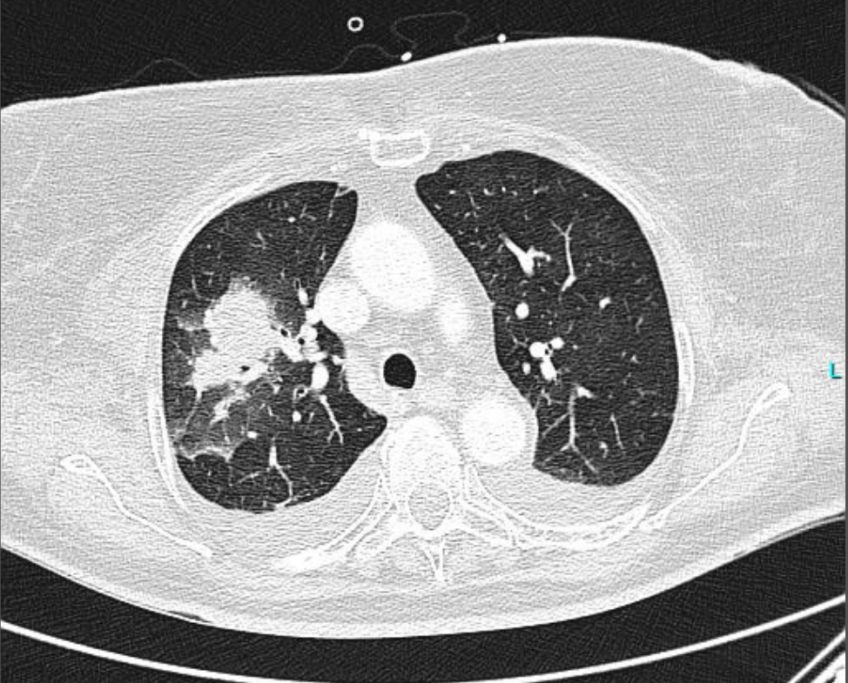
78 yo male, COVID+, worsening SOB. Recent hx: Transferred from OSH for worsening SOB, +CoVID 8 days prior to transfer.
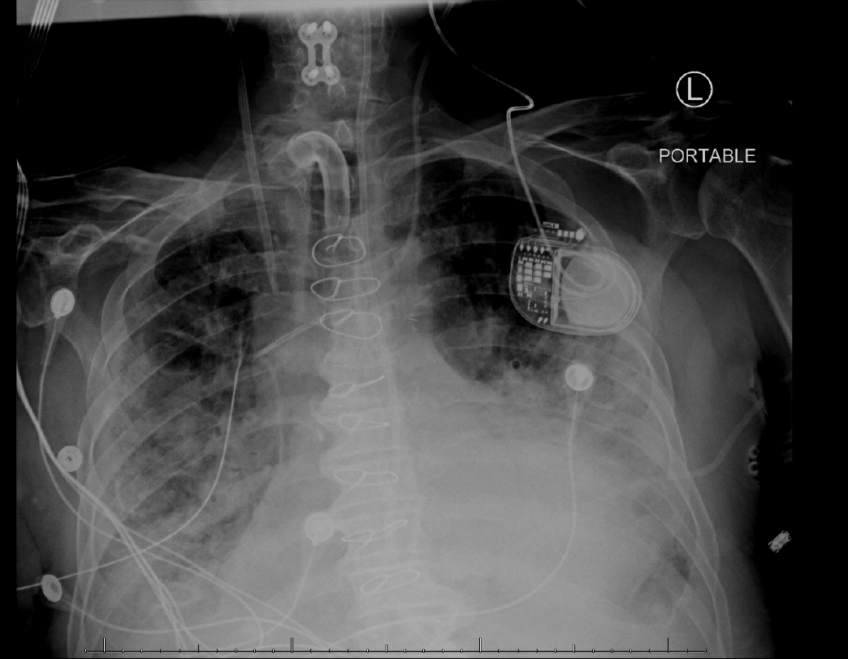
78 yo male, COVID+, worsening SOB. Recent hx: Transferred from OSH for worsening SOB, +CoVID 8 days prior to transfer.
Case #2: COVID-19 and Aspergillosis.
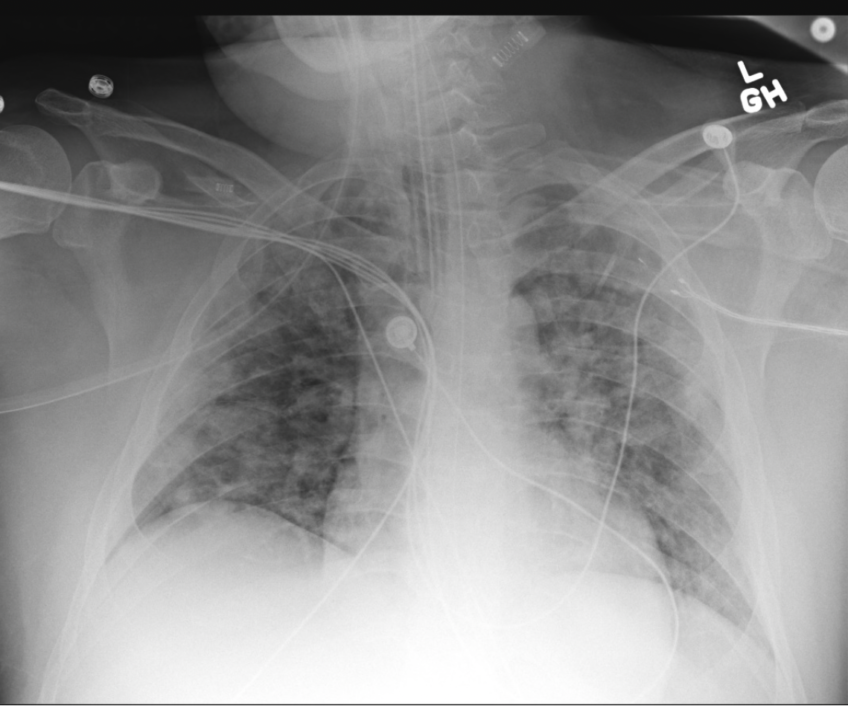
50-year-old male, shortness of breath, dry cough, fever and worsening hypoxia
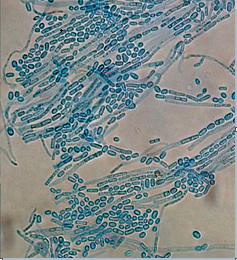
Case #1: COVID-19 and Pulmonary Aspergillus.
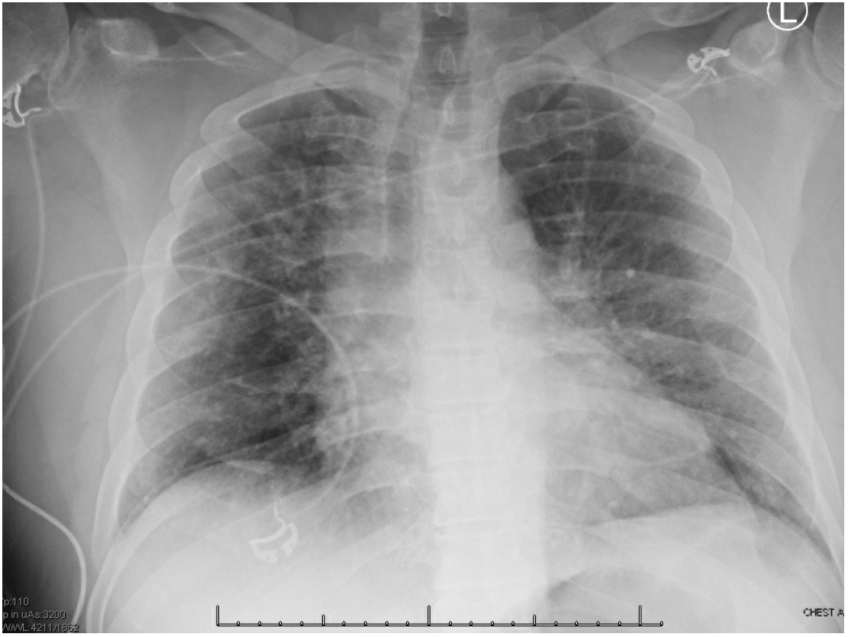
63-year-old male, presents with shortness of breath and positive SARS-CoV 2 (Covid).
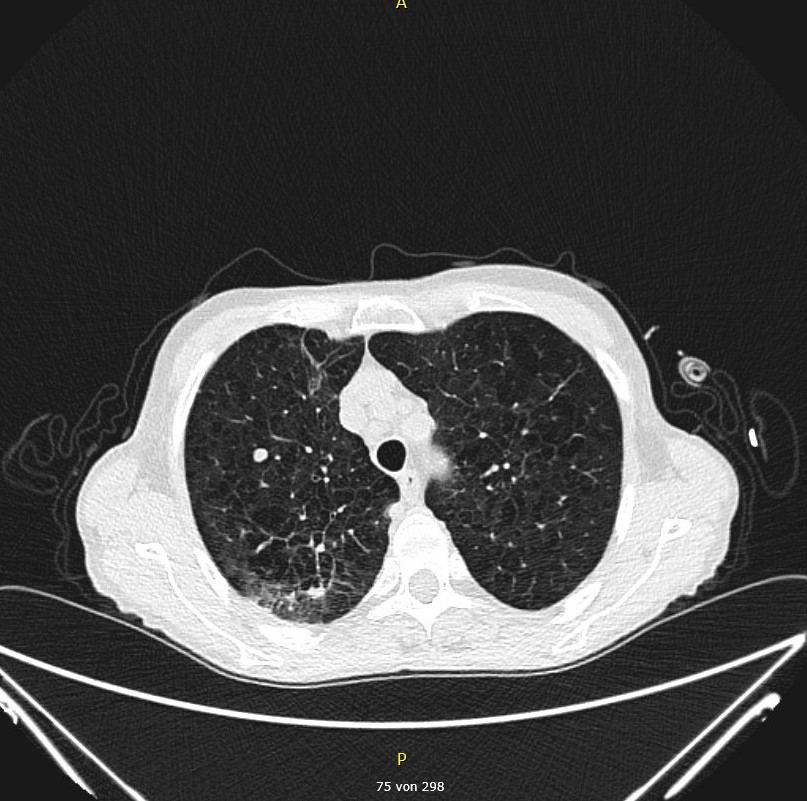
A 66-year-old woman presented with exertional dyspnea, leg edema, pretibial skin hemorrhages and subjectively perceived deterioration of her general condition. The medical history included hypothyroidism. The peripheral blood analysis at admission to hospital showed pancytopenia (Hgb 8.4 g/dl, WBC 3.03 x 10*9/l, platelets 28 x 10*9/l) as well as the presence of 46% of blasts. The results of the bone marrow puncture on the following day confirmed the diagnosis of acute myeloid leukemia (AML). The baseline CT of the thorax five days after admission to hospital showed a small round focus within the right lower lung lobe.

63 year old male, presents with shortness of breath and positive SARS-CoV 2 (COVID-19).

A previously healthy 63-year-old male with no significant PMH presented to the emergency department as a level 2 trauma transfer from an outside hospital after sustaining a tree trunk injury to his left lower extremity earlier in the afternoon, resulting in significant swelling.
A 59-year-old man was admitted with five days of diffuse body pain involving shoulders, arms, legs, chest, and back associated with fatigue and generalized weakness.
A 70-year-old female with acute myeloid leukemia (AML) and prolonged neutropenia, status post 5 cycles of azacitidine and venetoclax, presented to the emergency department with two days of swelling around the left eye and progressively worsening pain of the eye, especially with eye movement.
60 yo white male has experienced largely non-productive cough for over 2 years. He reports occasional sputum production and streaky hemoptysis. Has severe DOE with 20 yds walking before becoming SOB.
A 48-year-old female with type 2 diabetes mellitus and stage IV diffuse large B cell lymphoma complicated by secondary hemophagocytic lymphohistiocytosis (HLH) was admitted to a tertiary care center for management of neutropenic fever.

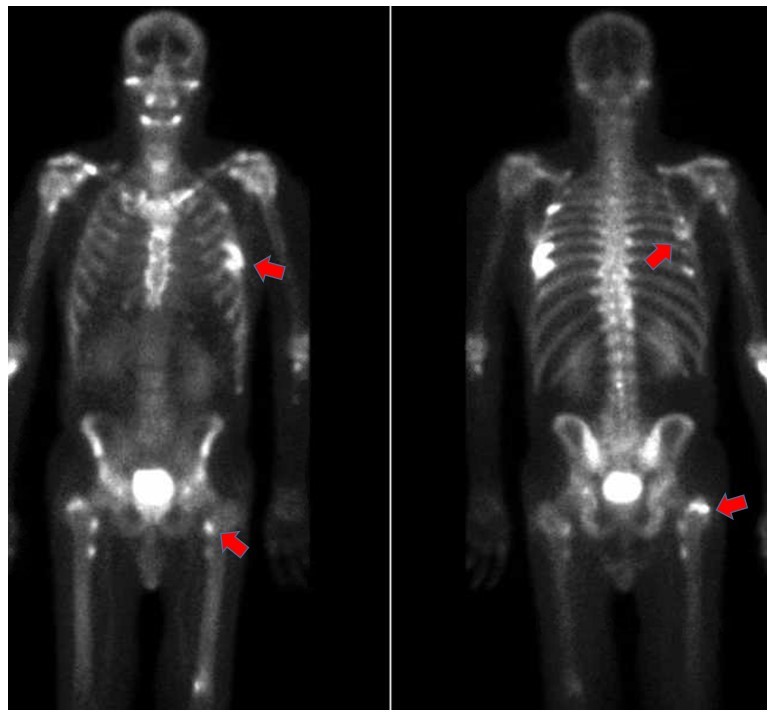
A 59-year-old male in-patient developed persistent fever and cough after 11 days of neutropenia following two cycles of chemotherapy for Hodgkins Lymphoma. The patient’s Hodgkins Lymphoma developed as Richters-Transformation (RT) from an underlying Chronic Lymphocytic Leukemia (CLL). The latter was treated with ibrutinib as third line therapy until the diagnosis of RT. During in-hospital treatment, the patient developed a skin-lesion on the left lower leg and, simultaneously, fever and cough.
A 57-year-old male with hypertension and hypercholesterolemia underwent tissue aortic valve replacement for bicuspid aortic valve. Six months later, he presented to an outside hospital with sudden acute abdominal pain and lower extremity pain and weakness. He reported a four-month history of right neck pain, and two months of low-grade fevers, sweats, malaise and dysphagia. He was born in Mexico and migrated to the United States 14 years prior. He lived in an urban area of South Carolina and worked as a landscaper.

A 75-year old women presented with fever and an unproductive cough which had been present for seven days. She had chronic lymphatic leukemia which was currently successfully treated with ibrutinib for almost one year.
A 40-year-old man brought to the emergency department by the EMS with altered mental status of 4 days, hypothermia, an area of pain and swelling on his left hand.
A 23-year-old man with Stage IV nodular sclerosing Hodgkin’s lymphoma was admitted with fever and erythema of his left leg that had not responded to standard antibiotic therapy.
A 68 year old male was admitted for ultrasonic lithotripsy. He had developed chronic renal stones in the setting of suprapubic catheter placement for neurogenic bladder. Subsequent recurrent urinary tract infections were managed with trimethoprim-sulfamethoxazole suppressive therapy. Medical history was notable for multiple sclerosis, and diabetes mellitus managed with oral hypoglycemic agents.
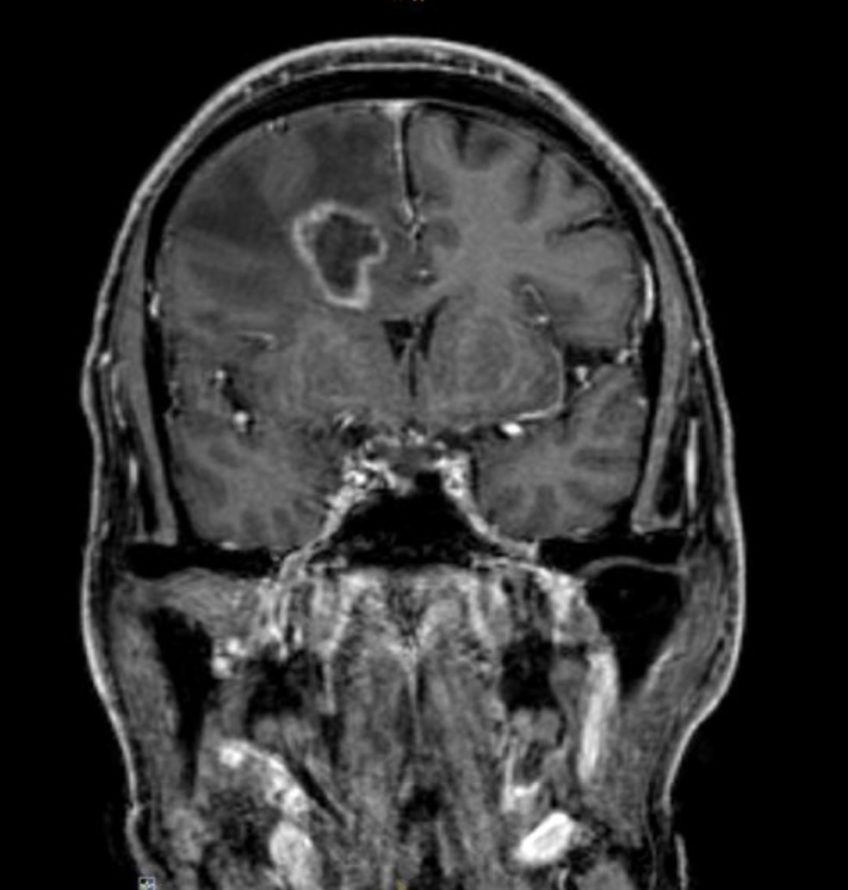
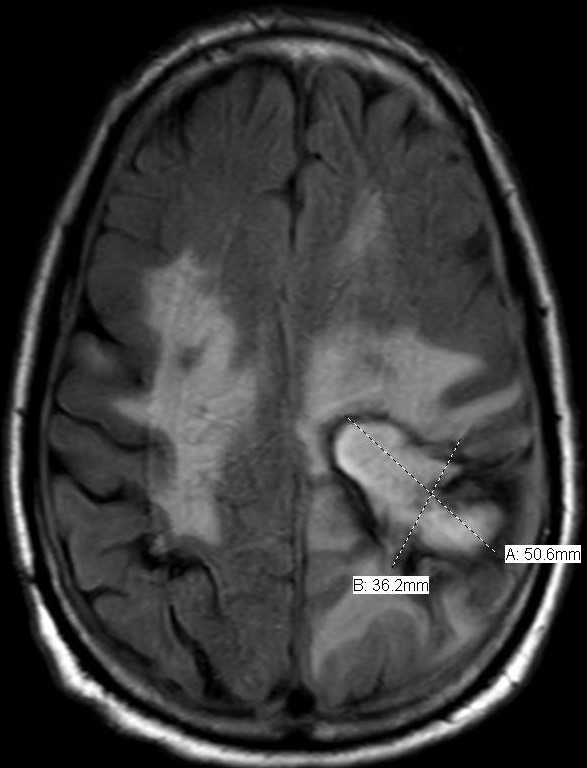
A 65-year-old man with FLT3-mutated and complex aberrant karyotype acute myelogenous leukemia presented himself in the outpatient clinic for follow-up after allogeneic stem cell transplantation. The patients’ wife reported a slight character change and memory loss over a period of one week.
The patient is a 66-year-old man whose cardiac history includes a coronary artery bypass graft performed 20 years ago, a bioprosthetic aortic valve placed 10 years ago, an intra-cardiac defibrillator (ICD) inserted 7 years ago, and ischemic cardiomyopathy.
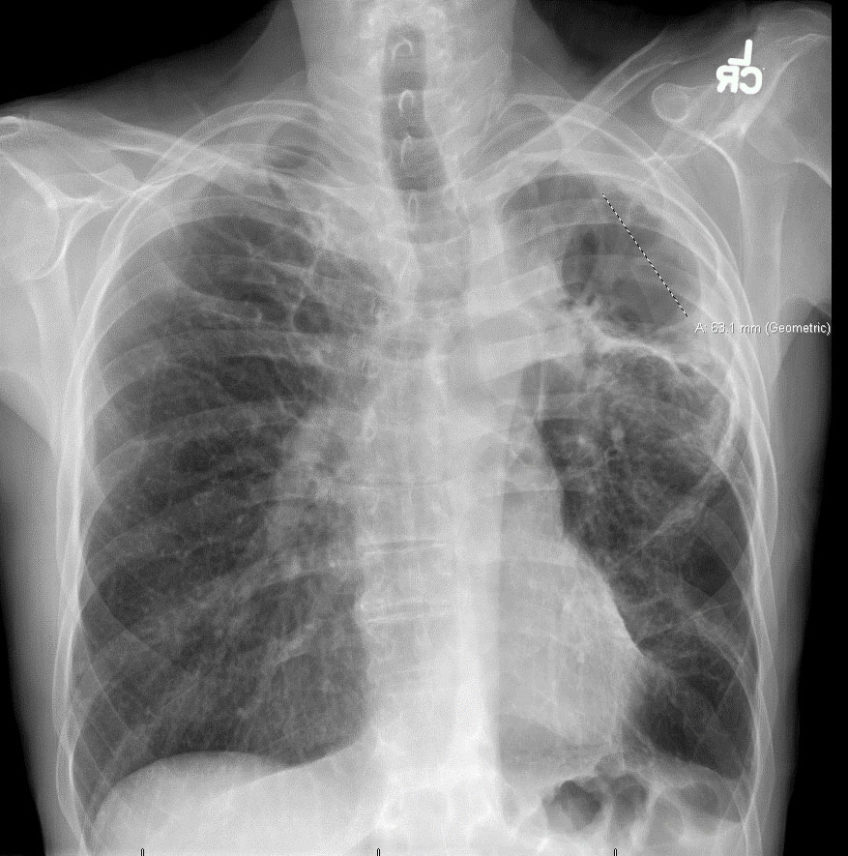
History: A 75 y/o woman was admitted directly to the intensive care unit due to vomiting and diarrhea. Due to repetitive hypertensive crisis, ectopic Cushing syndrome was suspected. The patient also had a steroid induced myopathy and diabetes. During her ICU stay she developed fevers and MRI was suspicious for intrapulmonary lesions that were described as chance findings and prompted a chest CT (Figure 1).
This is a case of a 24-year-old old woman with a history of uncontrolled type I DM, diabetic retinopathy, numerous admissions for diabetic ketoacidosis, and a recent HbA1C at 11.4 who was admitted for increasing left sided facial swelling associated with associated tingling, numbness and severe pain. Additionally, she also reported to have lost vision in the left eye about 3 weeks ago prior to her presentation. Patient stated that her symptoms started about one month ago after an infected left upper tooth which was subsequently extracted by her local Dentist.
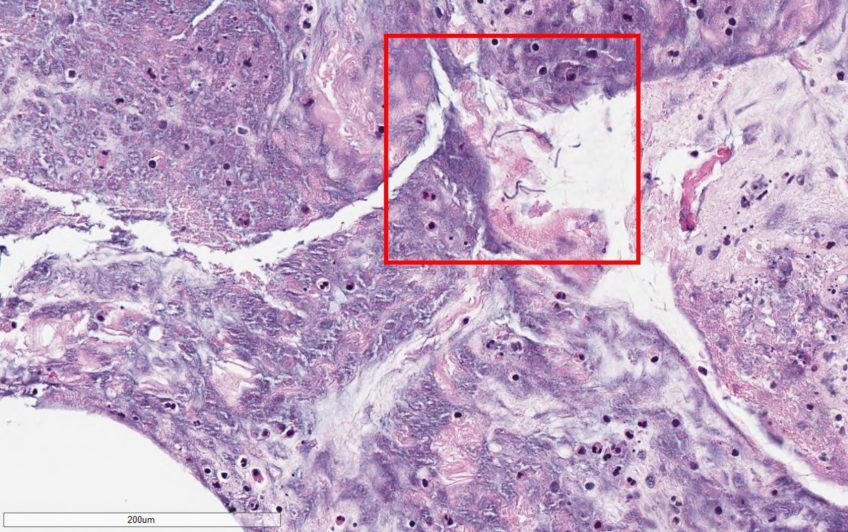
Skin lesions in a patient with acute myeloid leukemia presenting with febrile neutropenia Submitted by: Amy Spallone, MD; Dimitrios P. Kontoyiannis, MD, ScD, PhD, FACP, FIDSA, FECMM, FAAM, FAAAS Institution: The University of Texas MD Anderson Cancer Center Email: aspallone@mdanderson.org History: 40-year-old male admitted for fevers of one-week duration and neutropenia. His past medical history was significant for acute myeloid leukemia diagnosed one year prior, now relapsed and refractory to salvage chemotherapy. One month prior to admission at MD Anderson, he was admitted at an outside hospital for weakness and fevers. During that hospitalization, two nodular lesions were discovered on […]
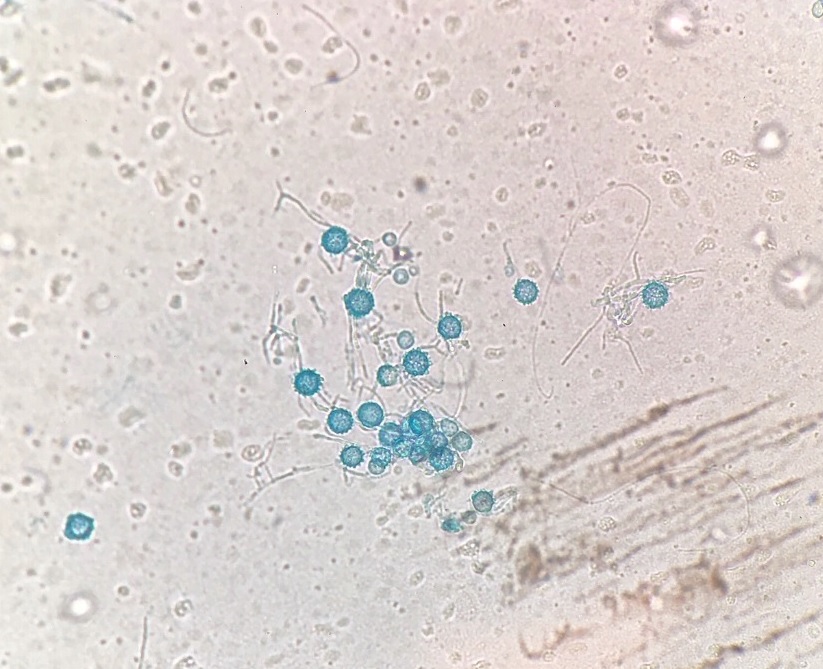
MSGERC Case of the Month Title: A Bold Mold Takes Hold Submitted by: Emily M. Eichenberger, Jennifer L. Saullo, John R. Perfect, Danielle Brander, Julia M. Messina Institution: Duke University Medical Center Email: Emily.Eichenberger@duke.edu Date Submitted: 9/30/2019 History: 62-year-old man with newly diagnosed chronic lymphocytic leukemia (CLL) on Ibrutinib therapy for 1 month prior to presentation with fevers, aphasia and a new brain lesion. He was doing well on the therapy for approximately 3 weeks until he developed a sore throat, and neck swelling. He was seen by an otolaryngologist who described a left peritonsillar abscess [Figure 1]. An […]
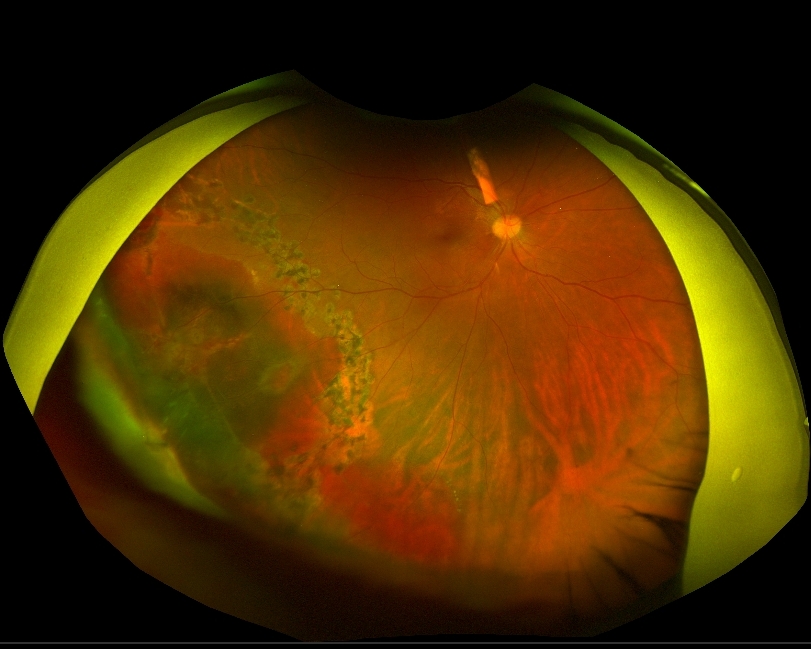
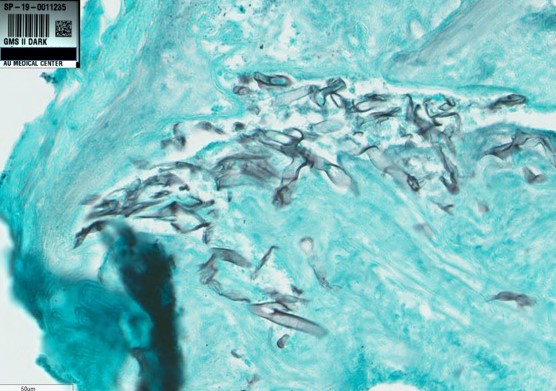
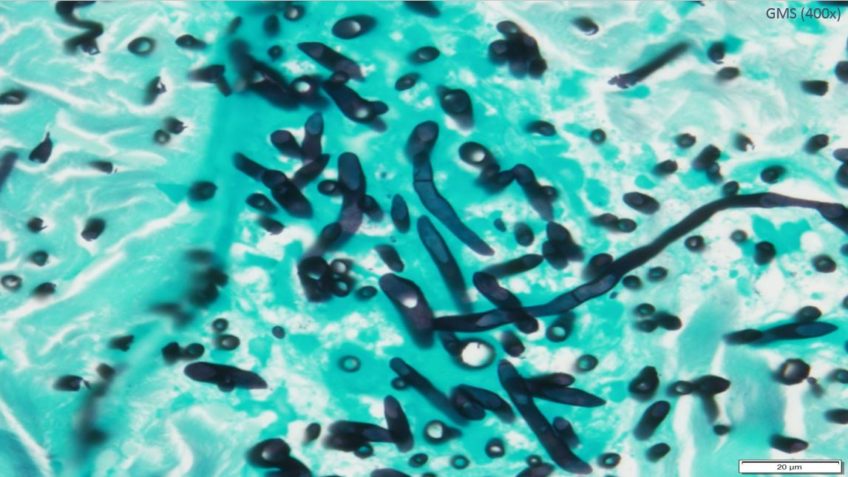
DrFungus.Org Case of the Month Title: Unilateral vision loss in a previously healthy patient Submitted by: Sarah Tran MD, Luke Chang MD Institution: Medical College of Georgia/Augusta University Email: satran@augusta.edu Date Submitted: 09/27/2019 History of Present Illness: A 30 year-old man presented to the emergency department with 3 weeks of progressive right eye pain and redness, accompanied by blurred and darkened vision in the affected eye. He denied any preceding trauma to the eye, fever, headache, or facial pain. He otherwise felt systemically well. He was initially diagnosed with uveitis and prescribed prednisolone and cyclopentolate eye drops by an outside […]
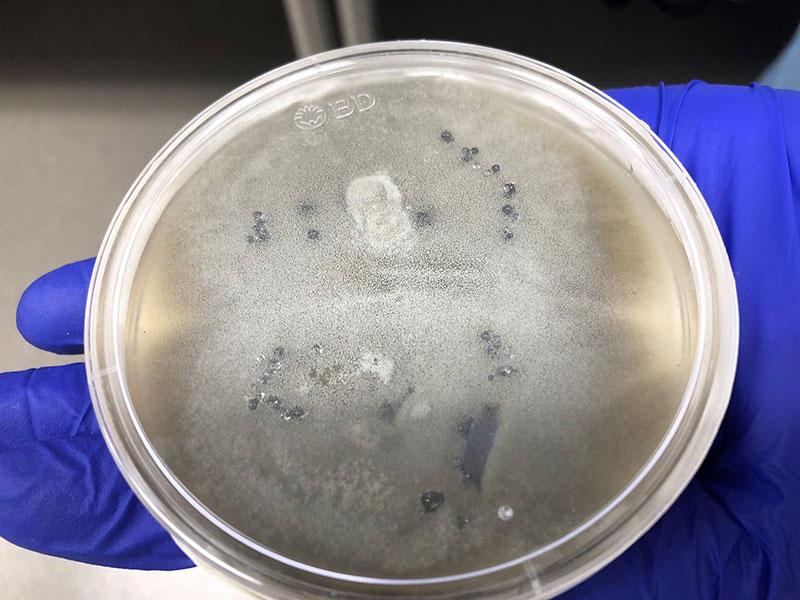
Centrifugal Fungus: Black Mold Emerges from the Tube Submitted by: Robert Rolfe Jr, Becky Smith, Jacob Klapper, John Perfect, Julia Messina Institution: Duke University History: A 67 year-old man originally from Colombia with end-stage interstitial lung disease was admitted to Duke University Medical Center (DUMC) for bilateral orthotopic lung transplant (BOLT). His BOLT surgery was complicated by hemorrhage requiring multiple units of red blood cells, plasma, platelets, and cryoprecipitate. Post-operatively, his chest was left open, and he was placed on veno-venous extracorporeal membrane oxygenation (ECMO). Per hospital protocol, the patient was placed on inhaled amphotericin B lipid complex prophylaxis as […]
Title: Fever of Unknown Etiology and Pancytopenia in a Solid Organ Transplant Recipient. Submitted by: Amy Spallone, MD, Laila Woc-Colburn, MD Institution: Baylor College of Medicine Email: amy.spallone@bcm.edu Date Submitted: April 2019 History: 34 y/o Hispanic male was admitted for worsening pancytopenia over the past two weeks. His past medical history was significant for alcoholic cirrhosis leading to orthotopic liver transplantation in August 2017. Two weeks prior to this presentation he was admitted for fevers without any associated complaints. He underwent an extensive infectious disease work up, which revealed he was Rhinovirus positive on respiratory viral panel. Patient was treated […]

Worsening Pneumonia, Intubation and ARDS Submitted by: Shiwei Zhou, M.D., & John Mills, M.D., University of Michigan History: A 78yo woman was admitted for ARDS in the setting of right sided pneumonia. About 3 weeks ago she developed fevers, chills, and a nonproductive cough. Chest X-ray at an urgent care showed a right lower lobe infiltrate, and she was started on PO Levofloxacin but worsened over the next 3 days. She was then admitted to an outside hospital and started on IV Ceftriaxone and Azithromycin, but continued to worsen over the next week with increasing oxygen requirements and was intubated prior to […]
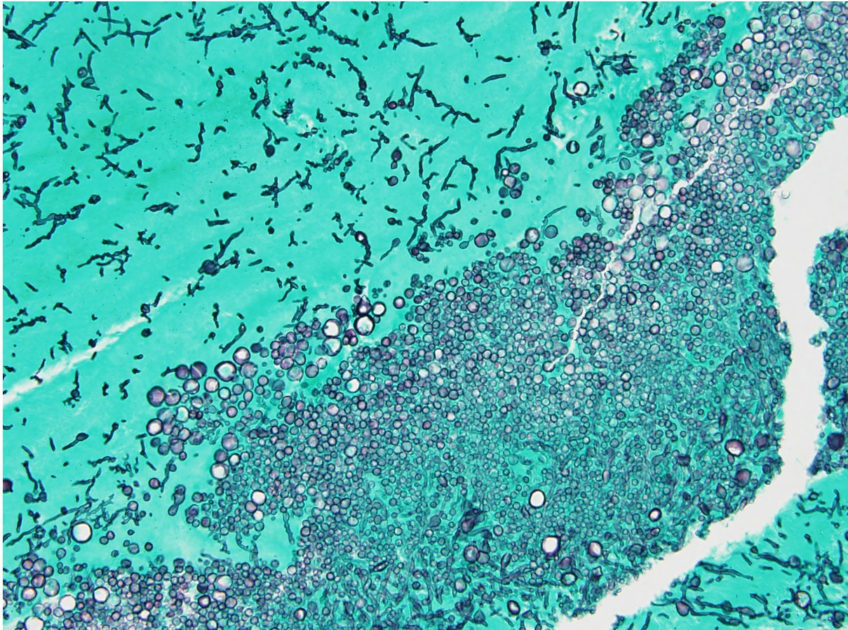
Progressive visual field loss, confusion, headache for 2 months Authors: Peter G. Pappas, 64 yo black male with recent onset of progressive visual loss on R visual field, confusion and headache. Symptoms have progressed over 2 months Until then the patient was in his usual state of health, no recent hospitalizations, procedures or history of trauma. Otherwise the patient denies fever, seizures, paresthesias, paresis, vertigo, or falls. Has a history of Evans Syndrome for which he takes low dose prednisone daily (10-20 mg/d) PMH: HTN Evan’s Syndrome Meds: Prednisone, Lisinopril, albuterol, HCTZ Social: From Birmingham, AL, no travel hx, no […]
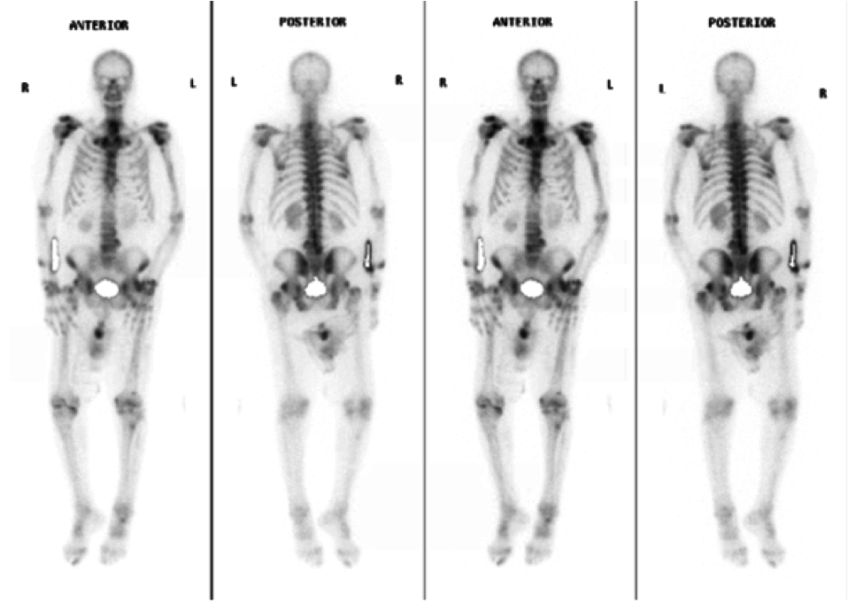
Authors: Melony Chakrabarty MD and Archana Maniar MD UC-Davis Medical Center A 70yr old Hispanic male with presents with history of disseminated coccidioidomycosis diagnosed in 2004 with progression of disease in 2016 with basilar meningitis requiring ventriculoperitoneal shunt. He has been on Voriconazole 200mg BID since June 2016, and has had therapeutic Voriconazole levels since 8/2016 (ranging 2.6 – 5.1). Admitted February 2018 for acute on chronic weakness occurring after a fall 2-3 months ago where he lost coordination and tripped over a table. Noted joint pain over L shoulder, L elbow and 2nd and 3rd L metacarpals. He describes […]

AML with persistent rash History: 23 yo woman with relapsed AML was recently admitted for re-induction chemotherapy. She became profoundly neutropenic and was managed with empiric antibacterial and antifungal therapy with micafungin. Despite persistent neutropenia, she remained stable afebrile on most days. On day 35 days following admission, she developed worsening fever and her regimen was changed from vancomycin, zosyn, and micafungin to empiric treatment with cefepime, daptomycin, and voriconazole. On Day 36, she developed worsening fever and a progressive palpable, painless, erythematous rash with lesions ranging from 1-2 cms. She remained febrile the on Day 37, with the development […]

History: A 79 y/o male with a history of acute myeloid leukemia on palliative chemotherapy (azacytadine) with persistent neutropenia (ANC < 100 over 12 weeks on prophylactic levofloxacin and voriconazole) presents with increasing pain over the right lower extremity. He states a raised “red” lesion developed over the last 2-3 weeks after he “bumped” against a park bench, and this area has progressively increased in size and pain. He additionally states the area of redness, swelling and pain has continued to increase as well. He sought care at an urgent care center and was prescribed a course of oral cephalexin for presumed cellulitis. Following this, his symptoms continued to worsen and he sought care within a nearby emergency room. He states since last seen the area of concern had formed a blister. He was started empirically on broad spectrum antibiotics with cefepime 2gm IV q8hr and vancomycin 1gm IV q12 and transferred to a tertiary care center. His review of systems was pertinent for subjective fever and chills, a scant dry cough, and shortness of breath with any exertion, but he denies all other review of systems.
If you would like to contribute a clinical case, please download the template and email us with jpeg images.
